Diet Advice, Health Trends & Informational Obesity
Obesity rates have been rising for decades. This trend has continued in very recent history, even though we aren't eating more or moving less. WTF is going on?
Not medical advice.
Diet Advice, Data & “Informational Obesity”
The USDA Food Pyramid and its consequences have been a disaster for humanity. This is not simply something we know due to the benefit of hindsight. The evidence upon which the foundation of The Pyramid was built was never “settled science,” a “consensus,” or whatever. It was cherry-picked by people with (often undisclosed) conflicts of interest. The Pyramid—which here means not just the literal Food Pyramid, but most of the guidelines promulgated by mainstream institutions like the USDA, AHA, and ADA—was designed by architects who had more than “the science” whispering in their ear.
I was born in the late 1980s. Growing up, I remember living through the “low fat” food craze. Everything was advertised as “low fat” or “fat free!” In grade school, the Food Pyramid was presented as the guiding star for nutrition. Constructed by the USDA based on evidence amassed from Experts, it essentially told us to eat:
Lots of carbs
Plenty of fruits and vegetables
Some dairy and protein-rich foods
Limited sweets

Later, he 1990s, I recall the Atkins Diet and low-carb craze. Despite the Food Pyramid’s emphasis on carb-rich foods, lots of people were apparently losing fat by cutting carbs. Diet fads come and go. It’s always been that way.
“Eat less fat to lose fat!”
“No, eat fewer carbs to lose fat!”
Endless cycles of dieting tips. Join Weight Watchers™. Buy the Oprah-endorsed book. Spend your money on this stuff, not that stuff. An ever-shifting cacophony of expert advice and nutrition secrets. Seed oil crusaders. Carnivore diet enthusiasts. Apostles of the Church of Veganism. Each claims to have it figured out.
Through all of the noise, a glaring constant: as a population, we keep getting fatter and less metabolically healthy.
This is all riding on a background of apparent knowledge growth. Every year, new studies pile up. There are more data points on metabolism and nutrition than ever before. Society is drowning in calories, data, and advice. It’s impossible to sift through it all on your own. In theory, we should be able to turn to the experts. But which ones? Everywhere you look, there are genuine experts—smart, knowledgeable people—who completely contradict each other when it comes to diet, nutrition, and human health. Very confusing.
Does this confusion stem primarily from a lack of information? Or is it possible that we’re suffering from information overload? A kind of “information obesity epidemic.” If the pattern of foods you consume shapes the obesity level of your body, might the pattern of information you consume shape the “obesity level” of your mind?
Better information comes from increasing signal and decreasing noise. Digesting yet another study does not guarantee better clarity. If it’s a good study, it provides signal. If it’s bad, it creates noise. And there’s a lot of noise out there. The scientific literature is not just voluminous—it’s contaminated with poorly designed, misleading, and even fraudulent studies. As we’ll see later, there are historical examples of well-done, insightful research that goes unpublished. There are also instances of cherry-picked results that go on to have a massive influence on research and public health policy.
We’ll evaluate new information when it comes and decide if it’s reliable. But we can boost our signal-to-noise ratio today, by sifting through what’s available and filtering out noise. A task of information curation, rather than data creation.
So WTF is going on when it comes to diet, obesity, and metabolic health? This is my attempt at some curation.
This article draws on information from these podcast episodes:
M&M #132: Obesity Epidemic, Diet, Metabolism, Saturated Fat vs. PUFAs, Energy Expenditure, Weight Gain & Feeding Behavior | John Speakman
M&M #131: Dietary Fat, Cholesterol, Cardiovascular Health & Disease, Carbohydrates, Dietary Guidlines, Food Industry & Diet Research | Ronald Krauss
M&M #115: Exercise Science, Nutrition, Plant vs. Animal Protein, Muscle Physiology, Sleep, Endurance vs. Resistance Training, Fat, Carbs, Amino Acids | Luc van Loon
Metabolic Health: Obesity, Diabetes & Metabolic Syndrome
What makes someone metabolically healthy vs. unhealthy? It depends on who you ask, but “metabolic syndrome” is generally defined as a cluster of co-occurring conditions. The exact diagnostic criteria may vary, but someone with metabolic syndrome will have a combination of:
Central obesity (excess body fat)
High blood pressure (hypertension)
High fasting blood sugar (insulin resistance / type II diabetes)
High blood triglycerides (a common form of fat)
Low HDL cholesterol (the “good” cholesterol)
These are all easily measurable symptoms that can indicate metabolic dysfunction—things going wrong at the cellular level. They all correlate with one another to some extent. Obese people are more likely to have insulin resistance (type II diabetes) than lean people, but it’s possible to have one but not the other.
If you have, say, three or more of the above, you’re likely to be diagnosed with metabolic syndrome—you’re clearly metabolically unhealthy. It’s possible to have one or two of these and be otherwise metabolically healthy. For example, a minority of obese people today are metabolically healthy—they do not have any of the other markers of poor metabolic health. Why? It’s basically because they have naturally higher levels of fat deposition, so their BMI is elevated for non-dietary reasons. (Note: this does not mean that obese is innocuous for some people. “Obese metabolically healthy” people are still at elevated risk for cardiovascular disease).
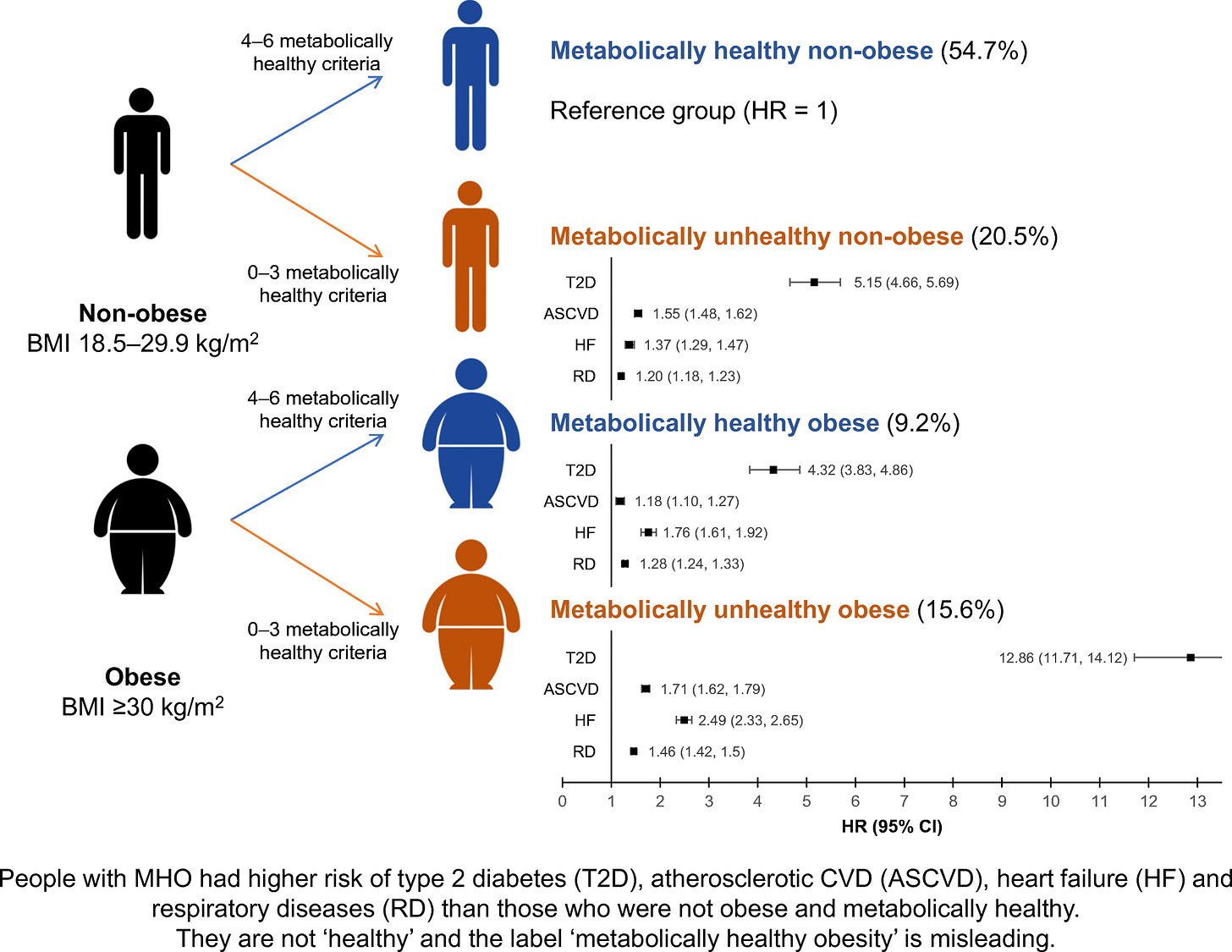
There are also non-obese people with metabolic syndrome. Even though they have a relatively low BMI, they have insulin resistance (diabetes), high blood triglycerides, etc. Each of the bullet points above is a potential outcome of poor underlying metabolic health.
For simplicity, when I refer to “poor metabolic health” or people who are “metabolically unhealthy,” let’s assume that means people with all five of the above. “Metabolically healthy” and similar descriptors will refer to people with none of the above. At times we will be talking about obesity per se or diabetes (insulin resistance) per se, but we’ll often be talking about general metabolic health. When I write about poor metabolic health, let’s imagine people who are obese, diabetic, and have all of those other symptoms. Indeed, this is the direction we’re drifting—every year, more and more people suffer from all of those things simultaneously.
Body Fat, Food Intake & Energy Dynamics
Over one-third of US adults are obese today, up from just over 10% in the mid-1970s. The obesity epidemic is commonly recognized as having started by about 1980. Since then, the rise in obesity in the US has been more or less constant.
If we’re getting fatter, it’s natural to suppose we’re simply eating more calories, moving our bodies less, or both. Over the long arc of human history, it’s pretty clearly both. Since industrialization, we have created a food environment in which foods are more calorie-dense, plentiful, and cheaper than ever. Consuming calories has become way easier over time.
We are also presumably moving our bodies (actively burning calories) less than our ancestors once did. We don’t live as hunter-gatherers or farmers anymore. For anyone who still engages in those types of activities, technology has made things easier, with fewer demands placed on the body.
What’s interesting is that obesity has continued to rise in very recent history, despite the fact that we haven’t continued to consume more calories. Since about 1999-2000, total available energy (how many calories we produce) and total calorie intake (how much we consume) have been flat. Despite this, obesity rates have continued to rise.

The obvious thought here is that we must be burning fewer calories. Perhaps we’re just lazier, not exercising as much. After all, technological progress has given us an endless supply of information and entertainment, cheap and easily available. Why lift a barbell when you can get all that by lifting your smartphone? It’s natural to suppose we’ve been moving our body’s less and less, allowing us to pack on the pounds even if we’re not consuming more calories than we were 1-2 decades ago.
But we aren’t moving less. In fact, evidence suggests we’ve been exercising somewhat more in the past couple of decades. CDC data indicates that the proportion of US adults who meet their physical activity guidelines went up from 1998 to 2018.
Other data, obtained from direct measurements of energy expenditure in humans, tell a similar story. Since roughly 1990, active energy expenditure—the energy we expend by actively moving our body (e.g. exercising)—has gone up, not down. Despite this, we’ve become more obese over the same time period.

So we continue to gain weight even though we’re actively expending more energy and eating about the same number of calories as we did in 1990. To understand what’s going on, we have to lay some groundwork:
Think about diet not merely in terms of total calories, but the specific macronutrient composition of what we eat—the pattern of specific fats, carbs, and proteins we’re consuming;
Understand how the macronutrient profile of our diet has changed over time, since the early 1900s;
Consider the metabolic effects that different macronutrient profiles have on our metabolism—the ways in which the food we consume influences how our bodies process it.
In other posts, we will consider the three main classes of dietary macronutrients—fats, carbs, and protein—focusing mainly on fats and carbs. This is largely because changes in protein intake have been much more stable over time. The pattern of specific fats and carbs we consume has been more dynamic.
One major lesson I’ve learned in studying metabolic health is that our metabolic dysfunction is downstream of insidious forms of information dysfunction.
To learn more about the topics covered in this essay, try these episodes of the Mind & Matter podcast:
M&M #132: Obesity Epidemic, Diet, Metabolism, Saturated Fat vs. PUFAs, Energy Expenditure, Weight Gain & Feeding Behavior | John Speakman
M&M #131: Dietary Fat, Cholesterol, Cardiovascular Health & Disease, Carbohydrates, Dietary Guidlines, Food Industry & Diet Research | Ronald Krauss
M&M #115: Exercise Science, Nutrition, Plant vs. Animal Protein, Muscle Physiology, Sleep, Endurance vs. Resistance Training, Fat, Carbs, Amino Acids | Luc van Loon
Related written content:





