Soy Foods & Cancer Drugs: Change Your Diet, Change Your Drug Sensitivity
New research links soy foods to liver metabolism, changing how the body metabolizes anticancer drugs.
Not medical advice.
Did your doctor carefully talk to you about your diet after prescribing you pills? Were you warned that eating grapefruit could make your more sensitive to your SSRIs? I have personally spoken to people on pharmaceuticals metabolized by CYP3A4 who had no idea that the fruit they eat affects the strength of the pills they take. Doctor never mentioned it—oops!
If this stuff is news to you, read this first.
The specific food components and drugs you ingest can affect the activity of key enzymes, rendering you more or less sensitive to other things, such as prescription or recreational drugs. This article covers the basics of cytochrome enzymes and provides many examples of foods and drugs that affect them. In some cases, food-drug and drug-drug interactions lead to dramatic changes, like this:
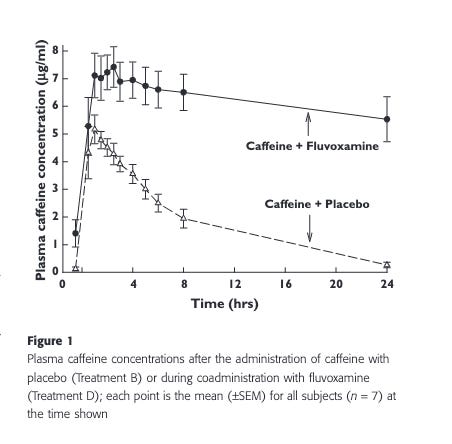
This post will briefly cover new research uncovering a previously unknown food-microbiome-drug interaction. In this case, diets with wildly different macronutrient profiles (e.g. ketogenic vs. high-carb) can lead to similar changes on anti-cancer drug metabolism, based on the presence of small quantities of a specific plant compound. The effect does not depend on macronutrients like fats or carbs. Instead, the gut microbiome can metabolize specific soy compounds, producing metabolites that then affect liver metabolism.
I’m not in the business of giving people medical or health advice (did you see the disclaimer up top?). I am in the business of connecting people with information and tools that can help them make their own decisions. The fact that you’re here and chose to read this far means you have some level of agency remaining. You aren’t like… the others.
Many people today are, unfortunately, living the life of Gollum from Lord of the Rings: addicted to the feeling of power emanating from the trinkets they carry, while their vitality is zapped by the artificial light, food, and drug environment they’re embedded in. The images on the walls of Plato’s Cave aren’t shadows cast by firelight; they’re now 4K images beamed onto your retina by blue LEDs.
Remember: although Gollum possessed the ring of power, he had no real power—just bad skin and a persistent cough.
Below, I will briefly describe results from a study linking soy compounds to drug metabolism via the microbiome. The larger point here is that the specific things you ingest, from “healthy” food components to pharmaceuticals, can drastically affect how your body metabolizes other things. Before describing the results of the new study, let’s briefly overview what’s already known about diet-drug-microbiome interactions.
Examples of Diet-Drug-Microbiome Interactions
The above study is just one interesting example among a growing body of literature on diet-drug-microbiome interactions. The gut microbiome can directly transform drugs, affecting their efficacy, toxicity, and how long they stay active, while diet shapes the composition and function of this microbiome, further influencing drug metabolism. This interplay helps explain why individuals can respond so differently to the same medication.
A short summary of the major forms that diet-drug-microbiome interactions can take, plus links to literature with examples:
Direct Metabolism: Gut bacteria produce enzymes that can activate, inactivate, or toxify drugs, altering their effectiveness and safety. Dozens of drugs are known to be directly metabolized by gut microbes, and in some cases, up to 70% of a drug’s transformation can be attributed to microbial activity (examples here).
Indirect Effects: Microbial metabolites can modulate the body’s own drug-metabolizing enzymes, further influencing drug breakdown and absorption. The example we covered above fits this mold. Other examples here.
Reciprocal Influence: Drugs can also change the composition and function of the gut microbiome, which may impact future drug responses or side effects. Examples here.
Diet-Drug Competition for Microbial Metabolism: Nutrients and dietary compounds can compete with drugs for microbial metabolism or alter microbial activity, impacting drug bioavailability and efficacy. Examples.
Learn more about the gut microbiome:
Podcast: Metagenomics, Microbiome Transmission, Gut Microbiome in Health & Disease | Nicola Segata
Podcast: Infant Microbiome & Breast Milk, Oral Microbiome & Cavities, Gut Health, Fiber, Probiotics, Diet, Sex Hormones, Soy Foods & Estrogens | Carolina Tropini
New study: Soy phytochemicals inhibit liver enzymes
From the introduction of this study, setting up some of the powerful ways in which diet can affect disease:
Dietary interventions can impact disease progression and drug responses. In preclinical cancer models, various diets have demonstrated the ability to slow tumor growth and enhance anticancer drug activity... A ketogenic diet has attracted particular attention for its ability to augment therapeutic responses, including in one of the hardest to treat cancers, pancreatic cancer. While a ketogenic diet on its own does not substantially affect pancreatic tumor growth in mouse models, it synergizes both with combination chemotherapy and with phosphatidylinositol 3-kinase (PI3K) inhibitors (PI3Ki), resulting in slower tumor growth and prolonged survival.
Elsewhere, I’ve covered the effects of ketosis and ketone bodies like BHB on everything from cancer to kidney function. In some cases, it has been shown that ketone bodies themselves are responsible for the effect studied. Because ketosis and ketogenic diets are now frequent objects of study, there are many interesting outcomes associated with ketosis that may not necessarily be driven by ketone bodies or the ketogenic state per se.
As this new study points out, the standard keto and non-keto laboratory diets given to experimental animals differ in ways other than macronutrient profile:
While standard rodent chow is made largely from unrefined foods (ground corn, soybean, wheat, and fish), a rodent ketogenic diet is made from purified components (e.g., oils and the milk-derived protein casein). Such ‘‘purified’’ rodent diets resemble processed foods that are pervasive in modern society. They differ from chow on multiple dimensions distinct from macronutrient composition, including digestibility and the presence of phytochemicals. When comparing diets that differ in multiple dimensions, it is necessary to figure out which aspects actually drive outcomes. A major but sometimes overlooked dietary factor is phytochemicals. Diets contain more than 26,000 distinct compounds, many of which might be bioactive and affect human health. Plants possess rich chemical diversity, containing phytochemicals such as flavonoids, terpenoids, alkaloids, and polyphenols. While certain phytochemicals have established bioactivities, research has focused on a small subset, leaving the vast majority of their potential effects unexplored.
[emphasis added]
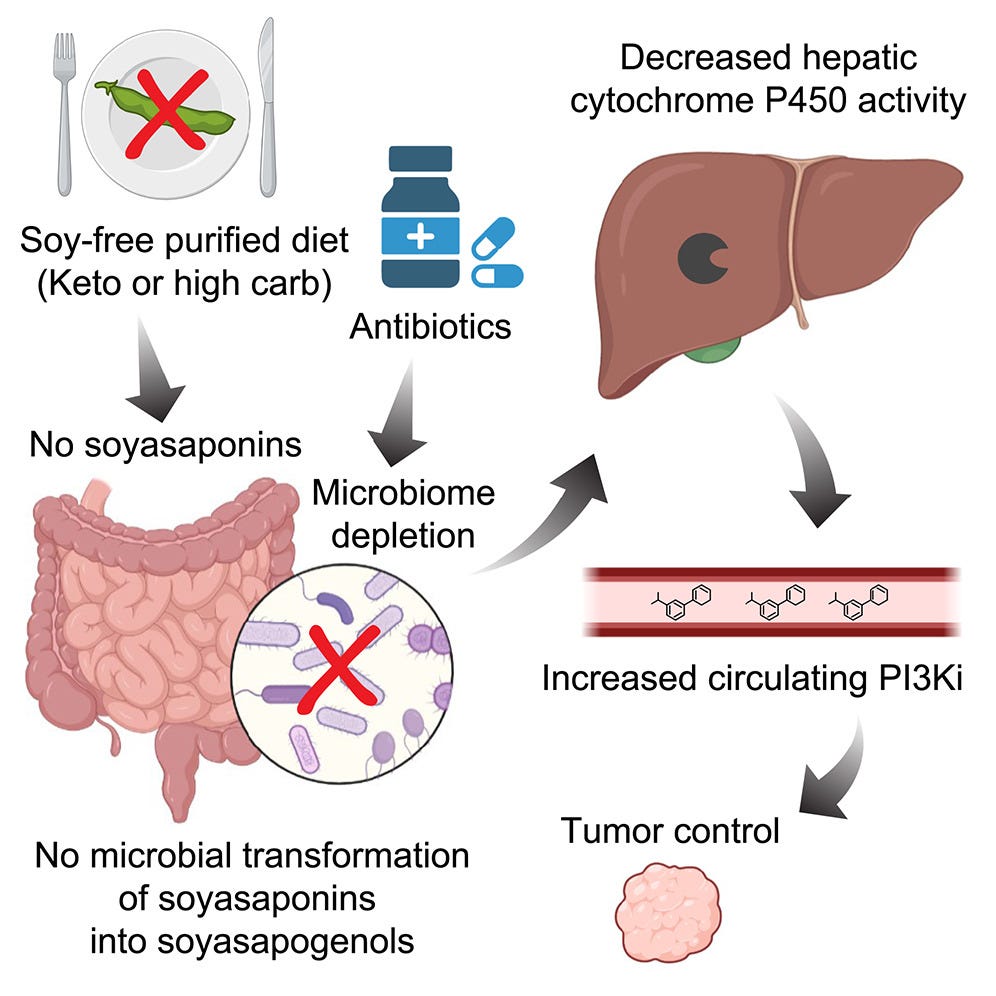
The graphical abstract of the paper, followed by a simple bullet-point summary of background information and key findings:
PI3K inhibitors are a class of anticancer drugs. It was known that rodent ketogenic diets synergizes with this type of drug to slow tumor growth and prolong survival.
It was presumed that the macronutrient profile of such ketogenic diets (high-fat, low-carb) was related to this effect, but this study showed otherwise.
Purified diets with any macronutrient profile tested (high-fat or high-carb) were able to enhance the anticancer activity of PI3K inhibitors. The anticancer effect had something to do with “purified components” of rodent chow, not macronutrients.
Microbiome depletion with antibiotics also increased the anticancer activity of PI3K inhibitors, indicating that the microbiome was the key to this diet-drug anticancer synergism.
The diet-induced enhancement of PI3K inhibitors on tumors resulted from higher drug levels, suggesting that perhaps some component of diet were affecting metabolism in a way that influenced overall drug levels.
CYP3A is an important liver detoxification enzyme responsible for breakdown of PI3K inhibitors in rodents. Purified diets or microbiome depletion (antibiotics) result in suppression of this enzyme, thereby boosting PI3K inhibitor levels.
Similar CYP-mediated metabolism is at work in non-human primates, suggesting it’s possible that human metabolism may also work this way.
Previous research showed that soy components can influence liver enzyme expression.
The driver of the anticancer drug synergism in this case was determined to be a soy-derived microbiome metabolite: soyasapogenol.
Basically, when fed soy-containing diets, gut microbes produce soyasapogenols, which are inducers of liver CYP enzymes. The presence of soy components in the diet leads to an enhancement of CYP liver enzymes that break down PI3K inhibitors.
Thus, ketogenic rodent chow and other “purified” rodent diets enhance the anticancer effect of PI3K inhibitors because they lack soy components, not because of their fat or carb content.

In other words, the effects of a “ketogenic diet” on anticancer drug activity had nothing to do with ketosis at all. Any “purified” rodent chow was able to drive this effect, which was also seen with microbiome depletion with antibiotics. For this effect, the key was that these purified diets were soy-free. In a sense, what was really going on is that standard rodent chow enhances the breakdown of PI3K inhibitors because it contains soy compounds.
Dose & Possible Effect in Humans
The standard mouse chow contained only contained 0.085% by weight of the key compound, soyasaponin Ab (SSA). Adding just 0.1% SSA or less to the purified diet reversed its effects on PI3K drug metabolism in a dose-dependent manner. In other words: the more soy, the faster the liver breaks down the anticancer drug.
As mentioned above, additional experiments indicated that something similar is at play in non-human primates, suggesting that things may work similarly in people (which remains to be directly tested). As the authors point out, “This 0.1% SSA dose is also comparable to the estimated dietary intake of group A soyasaponins in humans consuming a high-soy diet.”
Soy-based products have are heavily marketed and consumed today, often as “healthy” alternatives to animal-based foods. In reality, soybean oil and other soy products are cheap ingredients that food companies use to keep prices low and sales high. The cheapness of soy is comes from its enormous supply, driven by government-subsidized soybean production.
Many cancers are also on the rise. The study reviewed above raises some possible concerns for those eating high-soy diets, especially those who get cancers that might benefit from PI3K inhibitors.
In addition to soy compounds and their metabolites directly driving effects of liver metabolism and endocrine disruption, pesticides like glyphosate are widely used on soybean farms. Other research has recently shown that glyphosate can drive inflammation and neurodegenerative disease in animal models. Soy-based products may therefore pose a multi-pronged risk to health: soy compounds and metabolites that disrupt metabolism, plus pesticide residue and other contaminants.
Learn more about pesticides and soybean oil:
Article | Glyphosate, Choline & Brain Inflammation: What's in your salad?
Article | Eating Fat Like Never Before
What Does This Liver Enzyme Metabolize in Humans?
Given the the effects of this study depended on the effects of soy metabolites on the CYP3A11 enzyme, it’s worth know what other drugs this enzyme breaks down. The equivalent liver enzyme in humans is CYP3A4/5, which metabolizes a wide range of compounds. Here’s a short, partial list of what human CYP3A4/5 acts on:
Pharmaceuticals such as statins (e.g., atorvastatin), antifungals (e.g., ketoconazole), and immunosuppressants (e.g., cyclosporine).
Endogenous hormones like testosterone and cortisol.
Lipids, including some fatty acids and eicosanoids.
Because the key microbial metabolite of soy compounds identified in the study above worked by boosting the CYP3A11 in rodents, we would expect a high-soy diet to enhance the breakdown of these other things as well. In other words, assuming things work the same way in humans, people on high-soy diets would be less sensitive to the effects of drugs metabolized by CYP3A11 (such as the list above), compared to those on low-soy diets. High-soy diets would cause them to more readily metabolize these things.
Potential Effects of Soy-Based Foods on Testosterone in Humans
In this article, I covered the endocrine-disrupting effects of xenoestrogens, including the effect of soybean estrogens like genistein, which at high topical doses can induce precocious puberty in young girls. As described in that article, the structure of the estrogen receptor allows it to be activated by a wide range of synthetic and plant-derived compounds.
Testosterone levels in men have been plummeting for years, and the ubiquity of estrogen-like endocrine disruptors in the modern environment likely plays a role. The results of the new study above point to one more potential mechanism contributing to modern endocrine disruption and feminization: soy-derived metabolites that modulate liver enzymes responsible for androgen metabolism.
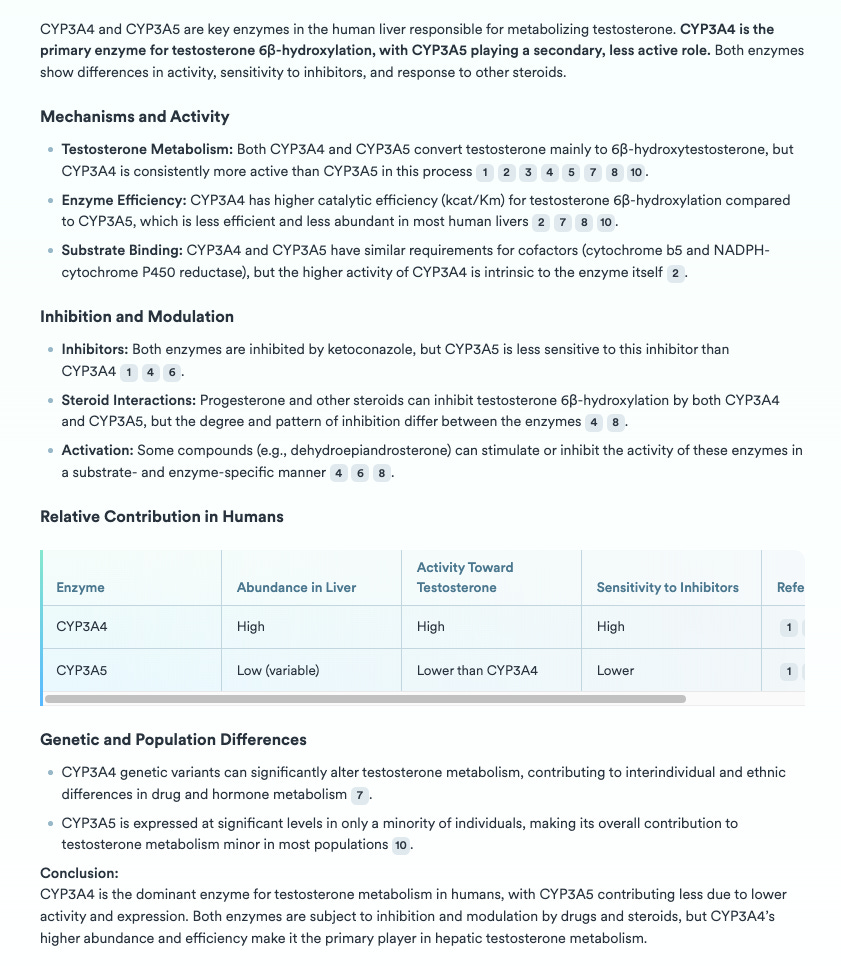
The equivalent enzyme in humans, CYP3A4, metabolizes testosterone. In humans, CYP3A4 is abundantly expressed in the liver and appears to be particularly sensitive to enzyme inhibitors, according to these studies. Here’s a AI-assisted summary of what the literature says about human CYP3A4 and testosterone metabolism:
To the extent that plant-derived xenoestrogens and related metabolites are altering androgen breakdown, this points to multiple ways, operating in parallel, they can drive systemic endocrine disruption in humans: Interfering with endogenous estrogen signals in the body; modulating the breakdown rate of other steroid hormones, like testosterone.
Think twice before you order your next latte, or buy a “healthy” plant-based protein bar.
Learn more about diet, metabolism and disease risk:
Article | Seed Oils, Early-Onset Cancer & Human Metabolic Variability
Article | Fructose, Corn Syrup & Cancer