Good Carbs, Bad Carbs: How good is "good" when it comes to insulin?
Some carb-rich foods are considered "good" and others "bad." How useful are these linguistic designations in reality?
Food & Insulin Resistance
Type II diabetes is a chronic metabolic condition in which cells of the body no longer utilize energy normally. Insulin resistance is a key component. Insulin is a hormone produced by the pancreas, important for growth and energy storage.
When we ingest foods that elevate blood sugar, insulin is released to promote absorption of glucose from the blood into tissues. The liver is a key site of glucose uptake. Glucose is primarily stored as glycogen (carbohydrate), but excess glucose that exceeds glycogen storage capacity can be converted to triglycerides (fat). In essence, insulin mobilizes tissues to store excess sugar, to be burned for energy later on if dietary energy sources run low. For wild animals facing scarce and unpredictable food supplies, this is a useful trick—hours, days, or even weeks can elapse between meals. Best to save surplus energy for later.
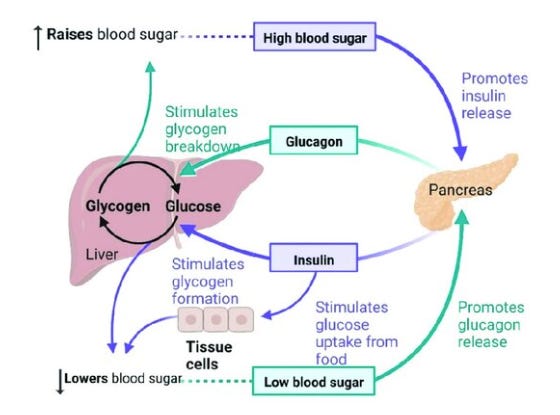
Food scarcity is rarely an issue for domesticated animals like modern humans. We have the ability to eat what we want, whenever we want it. Excess calorie consumption (positive energy balance) elevates insulin—the body’s hormonal signal that energy is plentiful and should be saved for a rainy day. If that rainy day never comes and you continue eating excess calories day after day, insulin remains chronically elevated and your growing energy stores never get burned—you get fatter.
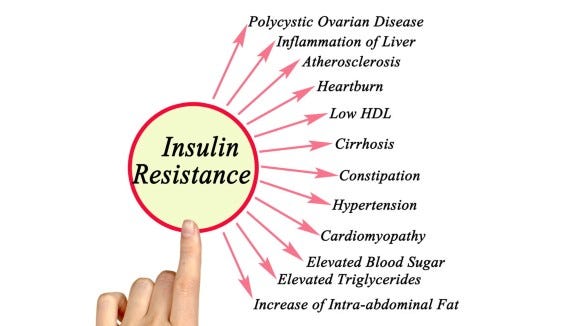
When insulin levels remain elevated for extended periods, insulin resistance can develop. This is not a terminal disease state. It’s an adaptive, reversible cellular response. Cells turn down their sensitivity to insulin when they have been over-stimulated by it—an attempt to compensate for excess insulin by decreasing their ability to respond to it. The problem is that this compensatory decrease in insulin sensitivity impairs glucose uptake. Cells become metabolically dysfunctional, unable to properly regulate glucose levels. A hallmark of diabetes is hyperglycemia—abnormally elevated blood sugar.
Compensatory responses like this are common in biology. Consider the phenomenon of tolerance in drug addiction. A low dose of, say, an opioid can elicit a strong physiological response. With repeated exposure, brain cells turn down their sensitivity to the drug (e.g. by reducing the number of opioid receptors). A higher dose is now needed to elicit the same effect.
Insulin resistance is not exactly like drug tolerance, but both involve the body adapting to elevated levels of a stimulus by reducing responsiveness to it. Excess insulin causes its own problems, but so does our cells’ adaptive response of limiting insulin sensitivity. Their ability to use energy to power normal, healthy functions is impaired, giving rise to problems that manifest as symptoms. Drugs can be taken to mask those symptoms, but reversal of insulin resistance requires removal of its cause: excess insulin, driven by excess caloric intake.
Eating too much food is (often) the cause of the problem. But not all foods are created equal. Different macronutrients stimulate different patterns of insulin release.
Insulin Release: Not all calories are created equal
The three major macronutrient classes—carbs, fats, protein—can all stimulate insulin release. In general, carbs stimulate more insulin release than fats and proteins. The simple sugar glucose is the most potent stimulator of insulin release. “Complex carbohydrates,” composed of many sugar molecules chained together (e.g. starch), get broken down into simple sugars by the body. This takes some time, causing a shorter peak in blood glucose and insulin, spread out in time.
Fiber, an indigestible complex carbohydrate, cannot be broken down to simple sugars by humans. This is why consuming carb-rich foods with high fiber content results in a blunted insulin response. Qualitatively, here’s how insulin levels respond to different carbohydrates: simple sugars (glucose), complex carbohydrates (starch), and complex carbs with high-fiber:
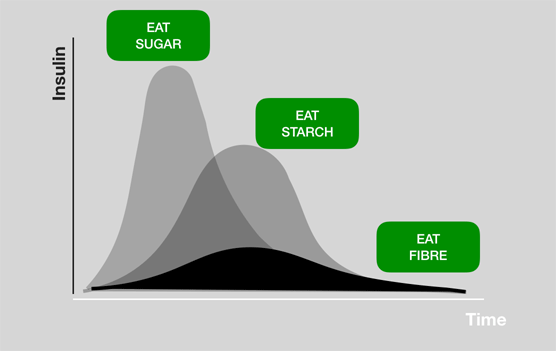
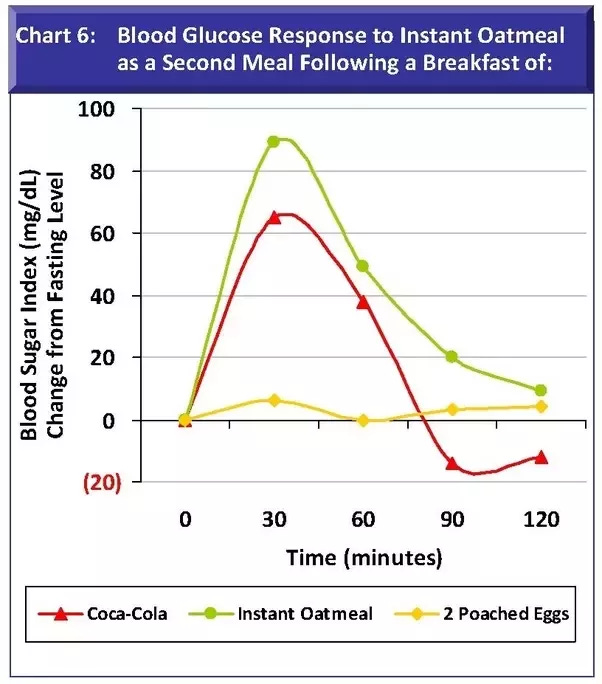
People often talk about “good” and “bad” carbs in terms of glycemic index, which describes the relative rise in blood glucose levels after eating. “Bad carbs” quickly turn into simple sugars, causing a rapid peak in blood glucose followed by a crash (high glycemic index). “Good carbs” have a lower glycemic index—peak blood glucose levels are lower, following a slower time-course. The patterns of insulin release will therefore be different for each.
Here’s some blood sugar data comparing Coca-cola to instant oatmeal . Notice that the coke causes a taller peak in blood glucose, followed by a crash. The oatmeal response has a lower peak but remains elevated longer. The total area under the curve, which will correspond to total insulin release, is actually comparable for each carb sources. Both differ dramatically compared to eggs, which contain mainly fat and protein.
Fat and protein can also raise blood sugar and insulin. Like carbs, it’s the smaller, simpler components of larger molecules that do this. With fats, triglycerides get decomposed into fatty acids. Proteins are broken down to amino acids. These simpler molecules can trigger insulin release. Unlike glucose, the blood sugar and insulin spikes are smaller. Moreover, glucose must be present for this to happen. If blood glucose levels are too low, amino acids generally won’t trigger an insulin spike. The amino acid leucine is an exception, which is why concentrated protein powders with high leucine content can trigger insulin spikes. Bottom line: fats and proteins trigger lower (and slower) insulin spikes than either “good” or “bad” carbs.

We are interested in insulin resistance, which is caused by too much insulin. In terms of macronutrients, carbs tend to cause the biggest glucose and insulin responses. But not all carbs are equal: some contain mostly simple sugars and little fiber, driving large insulin spikes and crashes (“bad carbs”); others contain complex carbohydrates and fiber, driving slower absorption and gentler fluctuations. How good is “good,” exactly?
Bread & Insulin: how good is “good”?
Here’s blood glucose data someone measured after eating a variety of bread types:

White bread clearly causes the biggest glucose spike. No surprise there—the other breads contain different combinations of protein, fiber, and resistant starches (complex carbs which break into simple sugars more slowly). More glucose means more insulin, so white bread is the worst option here for anyone trying to minimize insulin. In relative terms, we could call white bread “bad” and the others “good.” But are they really “good” or are they just better than white bread, which is terrible? That’s an important distinction, requiring us to look more closely at the relationship between blood glucose levels and insulin.
Unfortunately, the relation between blood glucose and insulin isn’t one-to-one. For example, it’s long been known that dietary glucose causes only slightly greater insulin rises than an equal amount of carbohydrate in the form of cooked starch. And doubling the dose of carbohydrate causes only small increases in the glucose response, but a larger change in insulin. For this reason, we need to look at insulin levels directly, rather than assuming blood glucose tells us exactly what insulin responses will be.
Here’s some insulin data from healthy adults (n=28) who ate two types of muffin tops matched for total carbs, sugars, protein and fat. One contained a resistant starch with fiber, the other did not:

As expected, the high-fiber muffin leads to less insulin release. However, insulin levels are still much higher for the control muffin than they would have been to a low-carb food rich in protein or fat. There’s no question that the high-fiber option is better for insulin control relative to the alternative. But is it a “good”? Should we recommend it to diabetics? Based on both common sense and the data on bread we saw above, it would be natural to recommend whole wheat breads over white breads to those with diabetes, right?
Let’s look at some more data, this time from a small group (n=11) of adults with type II diabetes. They ate different bread and had blood glucose and insulin measured. Here’s the glucose data:
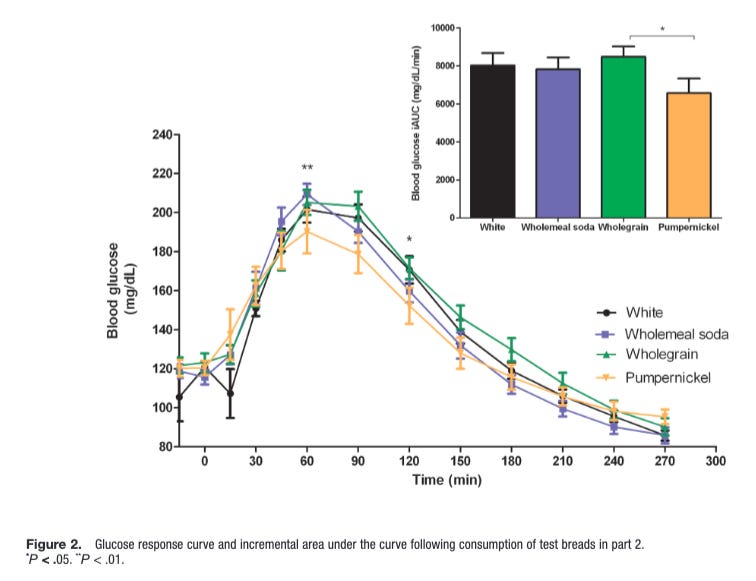
Small differences in blood glucose dynamics. Surprisingly, the white bread did not result in the biggest glucose spike. What about insulin?

Not what I expected. Wholegrain brain spiked insulin levels more than the others, including white bread. Also notice that the differences in insulin response are more striking than the glucose responses, further emphasizing why it’s important to look at insulin directly.
This result confuses me. White bread is supposed to be a “bad” carb, whole grains “good.” Is this result anomalous? Here’s data from another study of adults with type II diabetes (n=12). They ate 50 grams of bread across two meals, for four different bread types: 3-grain sprouted sourdough, whole-grain sourdough, white sourdough, and white bread. Naively, I would expect the glucose and insulin responses to be highest for white bread. The data:

There is no significant difference between any of the breads for the first insulin spike. For the second spike, the sprouted sourdough and whole-grain sourdough show only a modestly lower insulin peak than the others. In all cases, total insulin release is comparable across breads and far higher than it would be with a low- or zero-carb meal.
Good carbs, bad carbs: comparing carb-rich whole foods
Below is a result where blood glucose and insulin measurements were taken from n=8 adult diabetics across a variety of carb-rich foods. It’s from 1987, illustrating that these basic patterns have been known for some time.

Notice again that blood glucose is an imperfect proxy for insulin release. Straight glucose consumption led to significantly higher blood glucose levels than other foods, but this was not the case for insulin. Despite driving smaller blood glucose spikes, bread, oatmeal, rice, and potatoes drove comparable levels of insulin to glucose consumption. If “bad carb” is going to mean anything, it would refer to pure glucose. And yet, we often see comparable levels of insulin release to various carb-rich whole foods, at least in diabetes patients.
Here’s another study showing comparable insulin responses to consumption of five different breads, this time in obese men. Again, similar or even higher insulin spikes are seen in response to whole-grain compared to white bread. Whole grains are commonly said to be better for metabolic health and insulin sensitivity than refined grains. I don’t dispute that, but have been surprised at how modest differences in the insulin response are when they’re there. Oftentimes, they’re not. For example, this meta-analysis found no overall difference between whole and refined grains when it comes to fasting glucose, fasting insulin, or insulin resistance, despite other positive effects on post-meal measures of glycemic control.
The studies above mostly looked at people with metabolic conditions like diabetes and obesity. What about healthy adults? In this study of health adults (n=20), white bread caused a greater insulin response than two other types, although the differences were fairly modest. In this one, soft pretzels and rye, wheat, and sourdough breads all caused comparable insulin responses, not much lower than to glucose itself.
This meta-analysis compiled studies comparing whole to refined grains. It found that, in aggregate, whole grains tend to drive a lesser insulin response than refined grains. However, many of the individual studies compiled found no difference. Among other things, discrepancies between studies are likely due to the specific grain-based foods studied.
Other carb-rich foods, such as rice, seem to consistently result in lower insulin responses than grains. My goal here is not to provide a comprehensive map of how different carb-rich foods affect insulin release. I’m simply pointing out that many carb-rich whole foods, including grains, often produce insulin responses comparable to or only modestly less than pure glucose. This can include various whole grains, often considered “good carbs.”
It’s also important to keep in mind that dietary components can promote insulin resistance without causing significant insulin spikes. Unlike glucose, fructose does not drive significant insulin release. Nonetheless, meta-analyses have found that fructose facilitates insulin resistance in the liver, where it is selectively metabolized. (For more detail on how fructose affects the liver, see my conversation with Dr. Robert Lustig).
If our goal is to improve insulin sensitivity and ultimately reverse insulin resistance, then we want to reduce insulin. We don’t want to do reduce insulin a little bit. We want to reduce it a lot. Even though various “good” carbohydrates do indeed evoke a smaller insulin response than “bad” carbs like glucose and white bread, they still often produce a larger insulin response than low-carb foods rich in fat or protein.
Here’s data from a study that calculated an insulin index for a large variety of foods. Insulin responses were measured in response to energy-matched portions of each, and plotted relative to white bread (insulin score=100):
First, notice what triggered more insulin than white bread. Sugary candies come as no surprise, but this was also seen for yogurt, potatoes, and beans. High-sugar, carb-rich sweets like doughnuts and cookies were comparable to, or even slightly lower than white bread. Specific high-carb foods, like pastas and grain bread, had lower insulin scores.
The overall point: it’s often not obvious which foods are “good” vs. “bad” in terms of insulin response. As a general rule, complex carbs trigger less insulin than simple sugars, but the differences are sometimes much smaller than you might expect. Fiber also matters—all things being equal, more fiber means less insulin. Protein and fat tend to produce lower insulin responses than carb-rich foods of any kind, which is why eggs have one of the lowest insulin scores overall—they’re nutrient dense and low in calories, with virtually none coming from carbohydrates.
“Good” vs. “Bad” Carbs: Only one way to know
If there’s no surefire way to know exactly how much a given food will affect your blood glucose and insulin levels. In fact, the same foods can lead to distinct responses for two different people. How you consume them also matters—eating high-fiber or high-protein foods before more carb-rich foods during a single meal will generally blunt the glucose and insulin spikes triggered by the latter.
As we’ve seen, just because a carb-rich food has some protein or fiber in it does not mean it will lead to a substantially lower insulin response than something consisting mainly of simple sugars. This makes it very difficult to put much faith in pre-ordained labels like “good carbs,” often based solely on the fact that they contain some amount of fiber or non-carb nutrition.
At the end of the day, the only way to know how you respond to a given food is to measure your response. Continuous glucose monitors are one tool for doing this, giving you near real-time data on blood glucose levels. These are a useful tool not only for diabetes patients but for anyone motivated to get a handle on their metabolic health.

I’m in good metabolic health and once used a glucose monitor. With just one week of use, I learned a lot. For example, the food that triggered the largest blood sugar spike for me was a whole-grain breakfast cereal, marketed as a healthy alternative to other “sugary” cereals. Despite the “healthy” designation bestowed upon it by marketers, it contained high-fructose corn syrup as an ingredient, which is why is caused a dramatic spike in my blood sugar (followed by a crash).
It’s also advisable to get bloodwork done, including fasting glucose and insulin levels. As we saw, blood glucose responses are an imperfect proxy for insulin levels. I personally get bloodwork done every 3-4 months, using an at-home test. Metabolic dysfunction is a growing problem, with insulin resistance at the heart of it. I personally don’t place much weight on the sloganeering that food companies and diet “experts” use to promote their favored foods.
If you take your metabolic health into your own hands by monitoring it directly, you may develop a different kind of resistance—a resistance to the language games people play to get you to eat what they want.
To learn more about the topics covered in this essay, try these episodes of the Mind & Matter podcast:
M&M #134: Omega-6-9 Fats, Vegetable & Seed Oils, Sucrose, Processed Food, Metabolic Health & Dietary Origins of Chronic Inflammatory Disease | Artemis Simopoulos
M&M #132: Obesity Epidemic, Diet, Metabolism, Saturated Fat vs. PUFAs, Energy Expenditure, Weight Gain & Feeding Behavior | John Speakman
M&M #140: Obesogens, Oxidative Stress, Dietary Sugars & Fats, Statins, Diabetes & the True Causes of Metabolic Dysfunction & Chronic Disease | Robert Lustig







“If you take your metabolic health into your own hands by monitoring it directly, you may develop a different kind of resistance—a resistance to the language games people play to get you to eat what they want.”
Drop the mic Nick! 💯🙏💪
Well written, enjoyed reading this. Thanks for sharing this with us.