Eat Less, Move More?
The energy balance model cannot explain the dramatic rise in obesity, especially in a world contaminated with unavoidable obesogens.
Summary:
Energy balance (calories consumed - calories burned) is necessary but not sufficient for explaining observed patterns of obesity and weight loss in humans and other animals.
Not all calories are interchangeable and they do not merely serve as fuel. Different calories are handled in different ways by the body. What you consume influences how the body metabolizes what it’s fed.
The specific foods we eat, as well as exposure to environmental contaminants, can disrupt the hormonal profile of our bodies and thereby change how readily we store calories as fat. Food components and chemicals that promote obesity are “obesogens.”
It is becoming increasingly clear that animals can inherit the poor metabolic health their parents acquired during their lives. Animals can pass on metabolic dysfunction to their offspring via epigenetic mechanisms, even if they themselves were born metabolically healthy.
Genetics matter (a lot) for how your body will respond to a given diet. Substantial genetic diversity exists among people in genes that regulate fat metabolism and other processes important for metabolic health.
Related Podcasts:
M&M #140: Obesogens, Oxidative Stress, Dietary Sugars & Fats, Statins, Diabetes & the True Causes of Metabolic Dysfunction & Chronic Disease | Robert Lustig
M&M #145: Epigenetics, Hormones, Endocrine Disruptors, Microplastics, Xenoestrogens, Obesogens & Obesity, Inheritance of Acquired Characteristics | Bruce Blumberg
M&M #154: Evolution & Genetics of Human Diet, Metabolism, Disease Risk, Skin Color and Origins of Modern Europeans | Eske Willerslev
Obesity, energy balance & will power
There are more overweight and obese people than ever. I won’t bother citing statistics here. We can all see the obesity crisis plainly enough. Many have tried and failed to sustainably lose weight.
Why?
The default way people think about obesity, often without realizing it, is through the lens of the energy balance model, which views weight loss as a matter of calories consumed minus calories burned. If you eat more calories than you burn, you’re in positive energy balance (calories in - calories out > 0) and will gain weight. If you eat fewer calories than you burn, you’re in negative energy balance (calories in - calories out < 0) and will lose weight. It’s that simple.
Under the energy balance model, weight loss is primarily about whether you’re exerting enough will power to be in negative energy balance. Want to lose weight? Eat less, move more. Not working? Try harder.
Thinking about obesity strictly in terms of energy balance cultivates a certain attitude. If weight loss is all about exerting enough will power to get into negative energy balance, then the cause of fat peoples’ bodies is fat peoples’ minds. The solution to the obesity crisis is therefore: “Eat less, move more. Try harder!”
To be upfront, I actually have quite a bit of sympathy for this attitude. I know plenty of people who have not put in a reasonable best effort at managing their weight and metabolic health. In some cases, they openly state wanting to know how to lose weight without giving up their favorite desserts and sugary alcoholic cocktails (which they ingest on a near daily basis). There’s only so much sympathy one can have.
But there’s quite a number of people who swear that they have been eating less and moving more, but haven’t been able to lose weight. They’re not hard to find. Here’s one recent example:
She goes on to describe her exercise efforts, share Smart Watch data, etc. Most of us know people like this—they really did start exercising more and made a concerted effort to cut back on calories, yet still struggled to lose weight. Given that our ancestors were able to effortlessly avoid obesity for most of human history, we have to explain why weight management is so effortful in the modern world.
(The first thing I’d say to the woman above: “It’s great that you’re putting in this much effort and cooking at home. What are you cooking, and how do you prepare it?”)
Anecdotes match population-level data: we are moving more than we were in previous decades, while caloric intake has been flat. Obesity has continued rising despite this, opposite to what the energy balance model predicts.

How can this be? Two broad, obvious possibilities spring to mind:
Scenario A: Lots of people are mistaken—they think they’re eating less and moving more, but they’re not. The population-level data may even be off somehow—it’s not like we’re literally measuring every calorie that passes through people or that they burn. People simply need to eat even less. “Try harder,” is still the mantra.
Scenario B: The energy balance model is wrong, or at least incomplete. Weight loss is determined by more than just net calorie consumption. People should focus more on what they consume, not just net calories.
I’ll jump to the punchline now: Scenario A explains why some people fail to lose weight, but Scenario B provides a much better explanation for the obesity crisis. The energy balance model is incomplete. Important factors other than calories consumed vs. burned influence body composition: the macronutrient composition of foods, the hormonal profile of the body, and exposure to environmental chemicals which alter metabolism.
Alternative models of obesity exist. The key to real understanding lies in a more holistic view of obesity, arising from integration of these models. Energy balance is a core component of this integrated model (calories matter), it’s just not sufficient to explain obesity.
Some people really do fail to lose weight because they never go into negative energy balance. Again, I’ve met plenty of them. They will happily advertise the “extra steps” they’re getting in, or that they ate only half a slice of cheesecake for dessert. Many such people. Blunt advice may be warranted: try harder. But what if their brain can’t try harder to the same degree that yours or mine can? People are different. Brains are different. Some of this is inborn. Some of it is our environment, including the foods we’re been exposed to from conception, in utero, and throughout life (more on all that, below).
Those shouting “try harder!” are also competing for attention with another, increasingly vocal crowd: the “body positivity” movement. According to this philosophy, you can be healthy at any weight (you can’t). One faction is telling people to do more work while Cosmo smiles and says, “You’re healthy and sexy!” Whose messaging is going to be more attractive to the average overweight person? It doesn’t matter if Cosmo is wrong about human health—they’re in the business of selling ad space to cosmetics brands, not saving lives. (I haven’t checked: are their Ozempic ads in Cosmo yet?)
A compact summary of the key things I will cover in much more detail in the rest of this post:
The energy balance model of obesity is inadequate at explaining obesity. Chanting “Eat less, move more!” will not reverse or stall metabolic health trends no matter how loudly or frequently it’s repeated. There’s a lot more going on here biologically, including things that people quite literally cannot escape.
The hormonal environment of your body determines how readily it stores calories as fat. In turn, the specific things that go into your body—foods, prescription drugs, toxins—influence its hormonal profile and ability to metabolize other substances. How readily your body turns calories into body fat depends on your hormones and metabolism, which are influenced by everything from the nutrient composition of your diet to psych meds, birth control, and endocrine disruptors that may very well be in your tap water.
Our modern environment is contaminated with obesogenic, non-food substances—pesticides, microplastics, and other synthetics. All of us has been exposed to some extent, which affects how our body metabolizes calories by influencing key hormones, like insulin. The obesogenic effects of these substances can actually be passed to the next generation. This helps explain why some people get much fatter than others despite consuming similar foods, or why obesity and metabolic disease are rising among young children.
All of these environmental factors interact with your intrinsic biology. For better or worse, many aspects of your physiology are constrained by inherited factors that make you metabolically distinct from others. The genetic lineage you belong to influences how your body processes different nutrients, limiting which diets will be good for you within a given social and geographic context. There is no universal human diet, for weight loss or for optimal health.
Before describing the major scientific models of obesity and how they can be integrated, we need to think about evolution and natural variation in human cognitive traits.
Human Evolution & Cognitive Diversity: Why will power is not enough
A broad distribution of heights exist among people. We see it plainly. Our final height is the result of gene-environment interactions that play out over time. Genetic constraints limit how tall we could get, but the environment—namely, the quality of our diet—determines whether or not we reach that potential. Malnutrition in childhood stunts growth. Full potential requires proper nutrition. This is common sense, and reflected in patterns of height we see across the globe over time.
One indicator of just how bad the modern food supply has become is that people are getting shorter. In the early 1800s, Americans were considered among the tallest people in the world. Globally, average adult height peaked around 1980 and has been declining since. Its unthinkable that this doesn’t have something to do with our diet. As the “Western diet” has spread across the globe, it has brought with it so-called “disease of civilization.”
Although at different rates, virtually every demographic in society is becoming more metabolically unhealthy, indicating that something about the overall environment is off. It’s as if substances that promote metabolic dysfunction are seeping out of the fabric of society itself, with little room for escape.
This is not a novel historical phenomenon. At the dawn of agricultural society, newly sedentary farmers tended to quickly become shorter, with less robust skeletons and more disease than their recent hunter-gatherer ancestors. People’s food environment and way of life shifted faster than biological evolution could adapt—an environmental mismatch with negative phenotypic consequences, including smaller stature and poorer health.
“Overall, historical evidence suggests that actually, hunter gatherers were able to work much less to procure their nutrition—they enjoyed a lifestyle that was less stressful, [with] social support networks close to them. They had ample free time. They exercise more, and they actually live longer. As soon as people settled down and started growing crops, then what you see is, first of all, the nutrition worsens—they start losing the enamel of their teeth because their diet is now much poorer, they rely on grain or other crops. The average height dropped by about 10 centimeters and actually didn't bounce back until the beginning of the last century.” —Dr. Dimitris Xygalatas, M&M #75
Today’s environment is changing more rapidly than that of early agriculturalists, a process which accelerates due to the compounding effects of technology. The faster the rate of environmental change, the more our minds and bodies will be mismatched to their surroundings. Biological adaptation is slower than cultural change and technological innovation. Why is there a metabolic and mental health crisis? In a very real way: because we’re not meant for this. We’re hunter-gatherers with iPhones and Frosted Flakes, posting selfies in the Big City. Of course we’re sick.
When your body is mismatched to the environment it’s embedded in, what do you do? When you’re a child born into it, you just call it life—you’ve never known different, so it never occurs to you that something’s off. Even if you one day wake up and recognize the mismatch, then what? Abandon your current life and join a roaming band of your tribal kin? Maybe this is why people love Burning Man.

Another idea: change the world—get rid of all the processed foods, microplastics, and other toxins in the modern environment. Let me know when you’re done. I’ll be right here.
The only sensible strategy I can see: continually educate yourself about the consequences of your consumption. As you learn more, deploy behavioral changes. Through trial-and-error you can home in on the consumption habits and behaviors that improve objective markers of health (bloodwork), lead to visible improvements in your body (leaner, stronger), and make you feel better on a day-to-day basis (mental health). Given that our society contains an over-abundance of harmful consumables, this will often require subtractive effort—learning how to filter out of your diet those things making you sick, sluggish, and soft.
All of that requires some will power. What is “will power”? Our intuitive notion will suffice. It’s related to mental faculties like attention, planning, etc. We all know that will power is finite, not infinite. Like a muscle, it can be strengthened, weakened, overworked, and under-utilized.
But here’s the thing: mental traits related to will power display natural variation just as physical traits like height and muscle capacity do. Whether or not we were malnourished as children, some people are “taller” than others when it comes to mental capacities related to will power. As any parent can attest (and as the marshmallow test demonstrates), variation in mental traits is apparent from early age. This means we can’t expect everyone to just “help themselves” when it comes to navigating our poisonous food environment. This is doubly true, as one of the things our food environment poisons is the brain, impacting the very circuitry governing our sensitivity to tasty temptations.
How the modern food environment affects the brain
The food environment begins affecting our brains before we’re even born. In pregnant female rodents, a dietary imbalance of omega-6 and omega-3 fatty acids alters the development of the reward circuitry in their pup’s brains. Those mice are extra sensitive to palatable foods, resulting in overeating. This dietary fat profile, with much higher omega-6 fat intake compared to omega-3, is also a major feature of the modern human diet. There’s plenty of evidence that a human mother’s diet during pregnancy impacts her baby’s brain.
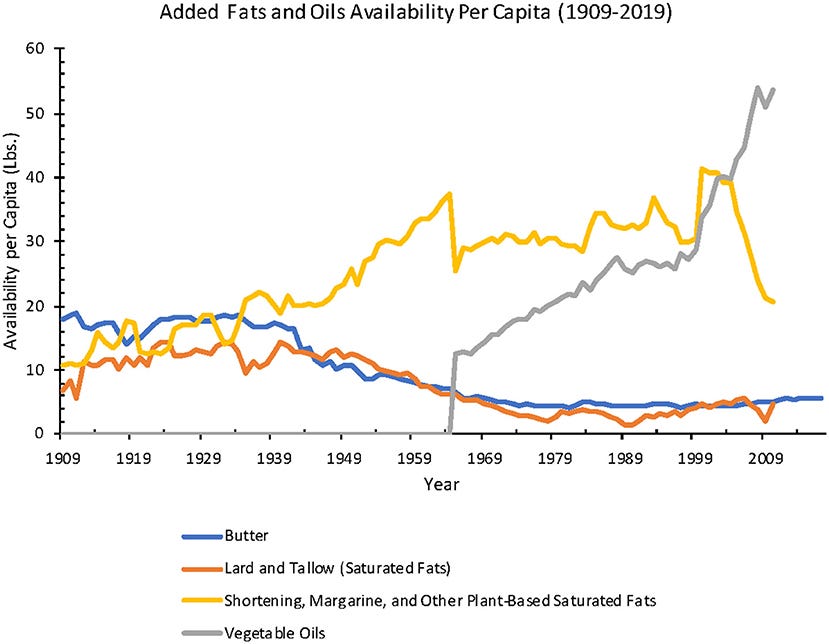
Modern humans have been consuming an excess of omega-6 fats for decades. This comes largely through the widespread use of industrial seed oils, found in most processed foods (including baby formula). As with rodents, a skewed omega-6:omega-3 fat profile is associated with all kinds of problems for the developing human brain. Drs. Chris Knobbe and Artemis Simopoulos have explained to me at length the myriad problems that arise from this kind of dietary imbalance.
If a poor diet during pregnancy and early childhood sculpts brain development in ways that make you more sensitive to food rewards, then you will be less able to heed the advice, “Eat less, move more.” The metabolic health of the next generation can influenced by the metabolic health of their parents at the time of conception. In addition to the natural variation in mental capacities, the industrial food environment we’ve been embedded in for decades has inevitably affected our brain development. An environment filled with literal poisons, neurotoxins and obesogens is leading to physical and mental degeneration. (What kind of culture springs forth from poisoned minds and bodies?)
Our volitional capabilities are modified by experience throughout life, after birth. The underlying brain circuits can be significantly re-wired through exposure to non-naturalistic stimuli. Drugs with high addictive liability, for example, cause unnaturally large releases of dopamine within the brains’ reward circuitry—they “hijack” it by stimulating neuroplasticity, re-wiring connections such that compulsive drug-seeking comes to dominate over natural, healthy drives. This doesn’t happen for everyone, but it happens for some. Natural variation is just a part of life.
Similar to synthetic or extracted drugs of abuse, ultra-processed foods can trigger supraphysiological responses in the brain. Food rewards tap into the same core reward circuitry (“mesolimbic dopamine system”) that responds to other rewards, which can be “hijacked” by addictive drugs. That’s why food addiction isn’t just a metaphor—much of our food supply has been deliberately created to be as addictive as possible. A team of PhDs engineered Flaming Hot Cheetos.
To the extent someone is truly addicted to food, telling them to, “Eat less,” isn’t going to be very effective. Maybe it would be for you, but you’ve got a different brain. I live in Seattle, a city filled with fentanyl addicts. How effective would it be for me to tell them: “You really need to try harder. It’s unhealthy. Here, check out these studies.” Are sugary desserts as addictive as synthetic opioids? Probably not. But you get the point.
“Eat less, move more,” requires having a brain receptive to the message and capable of carrying out the necessary behavior change. Due to both natural and environmentally induced variation, some people are more weak-minded than others. Even if we all had the same level of will power, there are other reasons why this mantra won’t solve obesity. To understand why, we need to look at alternatives to the energy balance model.
The major scientific theories of obesity
There are a handful of scientific models of obesity, each emphasizing different things as primary biological drivers. They are not necessarily mutually exclusive. Some researchers have proposed a new theory of obesity that takes into account what each of the other models does and does not explain, combing them into a new, unified theory of obesity.
I previously spoke to Dr. Robert Lustig about this new model of obesity. Below, I will briefly summarize what each of the four traditional models of obesity sees as a the fundamental driver of obesity, followed by an explanation of where they fall short and why new model, centered on obesogens and oxidative stress, was formulated.
Four models of obesity: brief overview
Below, a brief outline and of the major scientific models of obesity and how they differ. After that, description of the new unified theory of obesity that’s been proposed. For more technical detail and references, see this paper. For a simpler, verbal description of this stuff, see M&M #140.
Energy Balance Model: Overeating and sedentary activity are the causes of obesity. Consuming more calories than you burn drives weight gain.
To lose weight: Eat less, move more.
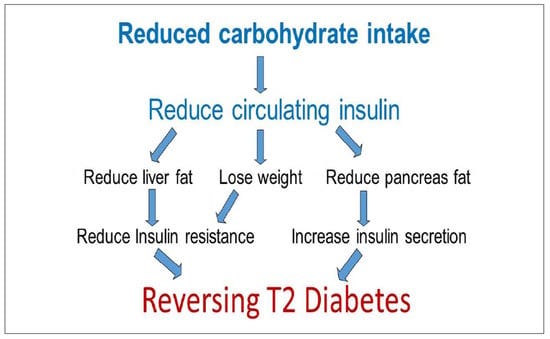
Carbohydrate-Insulin Model: Insulin drives energy storage (body fat gains). Different macronutrients drive different insulin responses. Carbohydrates drive more insulin than dietary fat and protein.
To lose weight: Restrict carb intake while moderating caloric intake.
Oxidation-Reduction Model: Reactive oxygen species (ROS, i.e. free radicals) damage the body, altering our metabolism. Energy surplus drives ROS production. Obesity arises from metabolic changes caused by oxidative stress.
To lose weight: Avoid foods and behaviors that promote oxidative stress.
Obesogens Model: Environmental chemicals interfere with hormonal signaling, promoting adiposity (body fat gain). Exposure to obesogenic compounds alters our hormones and metabolism to drive obesity.
To lose weight: Avoid foods and other products contaminated by obesogens.
The energy balance model is the oldest, stemming from the basic intuition that energy storage (body fat) is all about how much energy (calories) you consume. If you eat more calories than you’re body needs to operate itself, it will save the excess energy as fat for later. Obviously, the body does do this—it’s why we accumulate body fat in the first place, and why a starving animal will have less body fat than a gluttonous one. Like, duh.
But that’s not the whole story.
Again: energy balance is a crucial component of obesity and metabolic health—it’s just not sufficient to explain the obesity crisis, all by itself.
Shortcomings of the Energy Balance Model
Before going over what the energy balance model overlooks and where it breaks down, we first need to clearly state (again) that energy balance matters. Total calories matter. How much you eat and how much you move are obviously important factors in your metabolic health and whether you will gain or lose weight. Don’t forget that as we talk about alternative models and where this one breaks down.
A few areas where this model struggles: food restriction and exercise trigger compensatory metabolic changes in the body; pharmaceutical drugs and hormonal medications often lead to significant, persistent changes in metabolism and body fat composition; under specific conditions, weight loss can happen in states of positive energy balance, and vice versa; both captive and wild animals living in close proximity to humans are gaining weight.
If you want to skip ahead to the unified model, the main failure of the energy balance model is that it simply can’t explain why, since about the year 2000, obesity rates increased even though energy intake decreased and energy expenditure increased. The energy balance model predicts the opposite.
Compensatory metabolic responses to food restriction & exercise
Hunger and metabolism are homeostatically regulated. In mammals, food restriction normally leads to physiological changes aimed at energy conservation: decreased basal metabolic rate, hormonal changes, etc. If someone merely eats less of the same foods they have been eating, such compensatory changes can offset the reduction in caloric intake.
Similar idea for increasing activity levels through exercise—not only can this drive compensatory changes in metabolic rate, it stimulates hunger. After a hard workout, I’m ravenous. Exercise often intensifies food cravings, which is going to make it all the more difficult on someone already struggling with appetite control. People who start exercising more may even unconsciously reduce levels of non-exercise physical activity. Believe it or not, seemingly trivial movements like fidgeting can have significant metabolic effects. All of the little micro behavior patterns of your day, things you don’t even notice, add up. It’s difficult to get people to consciously change behaviors they’re largely unconscious of.

Obviously if you move more and starve yourself (e.g. through a multi-day fast), you will eventually burn off body fat despite any compensatory metabolic changes. But this isn’t reasonable, scalable strategy for the general population. The energy balance model struggles to explain the typical, motivated overweight or obese person who has made genuine effort—someone who has, say, cut their caloric intake 20% and started exercising more, running a mild-to-moderate energy deficit. While it’s true that some people are simply mistaken about how much they’re really eating and moving, we can’t dismiss everyone struggling to lose weight despite real effort.
Again: weight management used to be much less effortful, even for our very recent ancestors. If you look at old photos of crowded American beaches, from any time before about the mid-1970s, it’s difficult to find many obese people.
As we’ll see, alternative models of obesity can explain why someone would struggle to lose body fat despite cutting back on calories enough to be in mild caloric deficit: what they’re eating and what their bodies are exposed to matter, not just net calories.
Medications can alter biological “set points,” resulting in persistent metabolic and body composition changes
From psychiatric drugs to hormonal birth control, more people than ever are regularly ingesting exogenous, doctor-prescribed substances—many have metabolic side effects and lead changes in appetite, food preference, and body composition. Stable changes in body weight and composition can persist as long as the person is exposing themselves, even if their lifestyle is otherwise the same. It’s as if the chemicals their consuming have changed some of their set points—targets that the body somehow encodes to maintain, in order to preserve homeostasis. Parts of the brain like the hypothalamus play an important role here.
Think about body temperature: your body has cooling and warming mechanisms that automatically trigger when your body deviates from it’s temperature set point, such as sweating and shivering. Analogously, hunger and metabolic rate are dynamically regulated in order to maintain a stable body weight under given environmental conditions. For example, the amount of energy your body needs depends on how cold your surroundings are.

If exogenous, non-caloric substances like psychiatric drugs can alter body weight and metabolism on their own, it suggests that body weight can be influenced by more than just net calories. A major factor in the dramatic rise in obesity is that the environment, including the drugs we take, has altered the mechanisms governing our homeostatic set points. Some obese people might be obese, at least in part, because their “body fat set point” is out of whack. Like a damaged thermostat, perhaps they’re stuck on an un-naturally high setting. As we’ll see, there are many substances (“obesogens”) that alter how our bodies process calories, promoting obesity independent of caloric intake.
Weight loss despite high caloric intake, due to hormonal changes
There are a variety of conditions under which weight gain and loss can be observed despite negative and positive energy balance, respectively. These are exceptional, such as certain pathologies, but illustrate that the body can be put into metabolic states that defy the energy balance model. Medical conditions like hyperthyroidism, for example, can significantly increase metabolic rate, leading to weight loss despite high caloric intake. This happens due to abnormal hormone release, demonstrating that the hormonal and metabolic context of the body is an important determinant of how calories are used. As it turns out, certain foods and non-food substances can have exactly this type of effect on hormones and metabolism.
Non-human animals are getting fatter
Non-human animals that live near us are getting fatter, as are those we keep in captivity. Why would wild animals in urban environments gain weight while their counterparts living off the grid do not, even when both populations have more than enough food to survive? Shouldn’t they be “naturally” regulating their food intake based on energy needs? They’re animals.
Why are primates living in research colonies getting fatter? Feral rodents? I personally know people who have diabetic house cats.
These things are awkward to explain if body weight and metabolic health are chiefly about total calorie intake. They are much less mysterious when you understand that food composition—what we eat, not just how much—influences the hormonal and metabolic state of the body. Cats evolved to eat the raw meat, fat, and organs of freshly killed animals, not dry kibble made from soybeans and corn. Even matched for calories, these diets will induce very different metabolic states, with very different health consequences.
Alternative models of obesity
The energy balance model is inadequate because it fails to take into account metabolic states, the overall profile of your internal milieu. Our individual metabolic states shift hourly, weekly, and across the lifespan. As with anything else in biology, complex gene-environment interactions dictate how this transpires. The current metabolic state you’re in governs how your body processes what you ingest. A major factor in determining our metabolic state is the types of calories we’ve been consuming, not just how many.
The carbohydrate-insulin model recognizes this, emphasizing the key role insulin plays in fat storage. Insulin is peptide hormone secreted by the pancreas. It’s an anabolic hormone, meaning that it stimulates the body to “build up” rather than “break down.” It’s most famous for regulating blood sugar levels. Many metabolic disorders, such as diabetes, involve deficits in insulin sensitivity. When insulin levels are high, you can think of it as being a general signal telling the body, “We’ve got plenty of extra fuel. Let’s store some up for a rainy day.” It promotes energy storage, i.e. adiposity (fat gain).
Unlike the energy balance model, the carb-insulin model focuses on the endocrine (hormonal) response of the body to its diet, rather than the caloric content of food. Two basic observations that influenced the model: (1) carbohydrates drive insulin release more than dietary fat or protein; (2) the obesity epidemic in the US coincided with adoption of low-fat fat diets that the US government began promoting in the 1970s. By and large, Americans listened. Food manufacturers followed suit, releasing a deluge of low-fat, carb-rich processed foods. This is clearly seen from analysis of food supply data, which Dr. Orrin Devinsky has explained in detail.
The basic idea of the carb-insulin model is that obesity and diabetes skyrocketed because people followed the advice illustrated by the infamous USDA food pyramid and parroted by physicians and medical institutions—they swapped fats for carbs, without reducing total caloric intake. Doing so naturally caused more insulin release, which promoted adiposity (fat gain) and insulin resistance, driving obesity and diabetes rates up and up. Pretty straightforward and logical.

The energy reduction-oxidation (REDOX) model emphasizes the role of mitochondria in generating energy from calories. As a consequence of ATP production, mitochondria generate reactive oxygen species. When energy needs have been met but fuel is still available, elevated levels of reactive oxygen species serve as signal for fuel storage (fat gain). In a state of frequent or persistent positive energy balance, the production of reactive oxygen species can exceed the capacity of the body’s natural antioxidant systems to quickly remove them. Cellular damage results. Over time, metabolism is disrupted in ways that promote obesity and metabolic dysfunction.
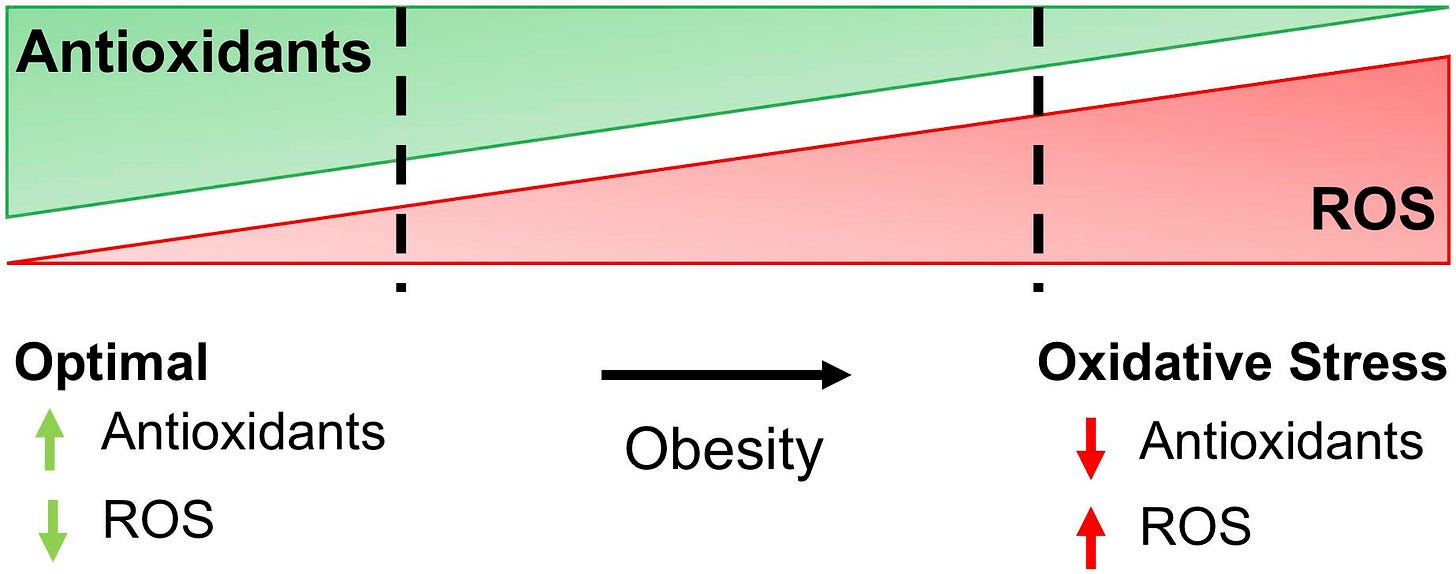
People with obesity and those who consume large amounts of ultra-processed food tend to have lower antioxidant capacities. They are therefore expected to accumulate more damage from oxidative stress. Individual fat cells from obese people are larger than those of non-obese people, usually showing signs of chronic inflammation and oxidative stress. Excessive body fat accumulation can further promote reactive oxygen species production. The basic idea is that obese people have more or less entered into state of perpetual oxidative stress, which disrupts metabolism. Among other things, oxidative stress can affect hormone secretion, gene expression, and energy homeostasis—a potential explanation for how someone’s body can get “stuck” at a maladaptive homeostatic set point, hampering efforts to alter body composition through calorie restriction and exercise.
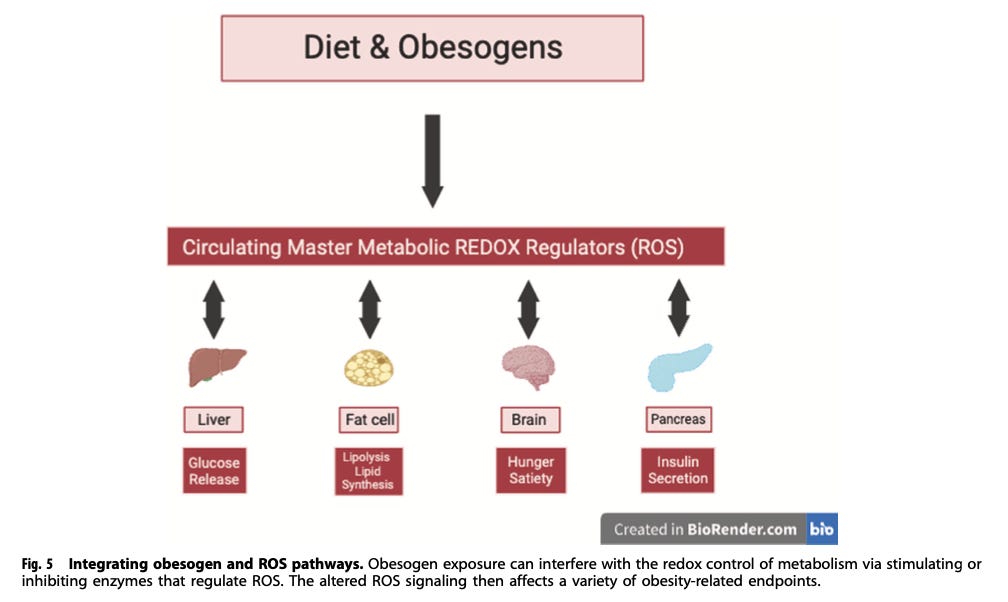
Lastly, there’s the obesogen model, which states that obesity is primarily driven by ingested or internalized chemicals that increase adiposity. There are both food and non-food obesogens, some of which we know we’re consuming, some we’re unknowingly exposed to. This model says that our whole environment, including our food supply, is contaminated with chemicals that directly or indirectly promote obesity in myriad ways—fat people aren’t just eating too much because there’s a surplus of palatable food, they’ve been poisoned.

Energy balance and total caloric intake still matter under these models, which are not mutually exclusive with one another. Each goes beyond mere calorie consumption, emphasizing different (but interconnected) aspects of biology in an attempt to explain metabolic dysfunction based on how our metabolism is altered by what we’re exposed to. Obesity and metabolic health are not simply a matter of net calorie consumption—the specific compounds that enter your body, and how they impact the regulatory mechanisms of your metabolism, are crucial.
The essential difference between the energy balance model and these alternatives can be grasped my imaging two identical twins living together, each consuming diets with equal caloric content but different ingredients. The energy balance model says they will experience the same amount of weight gain or loss. The other models say that their metabolic health, including their weight, will diverge over time.
A new unified theory of obesity?
In their own words, here’s how the authors of this paper describe their unified model of obesity:
“We propose a combined obesogen/REDOX model in which environmental chemicals (in air, food, food packaging, and household products) generate false autocrine and endocrine metabolic signals, including reactive oxygen species, that subvert standard regulatory energy mechanisms, increase basal and stimulated insulin secretion, disrupt energy efficiency, and influence appetite and energy expenditure leading to weight gain.”
In other words, exposure to obesogenic chemicals in our environment results in disruption of the control mechanisms that regulate reactive oxygen species (ROS) production. This messes up metabolism in ways that promote weight gain. When this happens, you could experience weight gain even under conditions where you previously did not. Disrupted ROS signaling can impact how the brain detects the body’s state of energy balance to drive hunger, how much insulin is released in response to carbs and other foods, how much fat our adipose tissue stores, and so on.
Think about it by analogy with the weight gain many people see when taking certain prescription drugs. An exogenous chemical is introduced to the body, instigating various physiological effects based on its mechanism of action. This can result in some set of changes in the brain and/or body that result in weight gain as a side effect. There are many ways this can happen. In the case of a prescription drug, we are intentionally consuming a biologically active compound with a known identity, which happens to have metabolic side effects. In the case of obesogens, we’re mostly clueless about our exposure to them.
Obesogens are everywhere—in the food, the water, and various household items—so ubiquitous it’s practically impossible to avoid them completely. Depending on where you live, there may be endocrine disruptors like tributyltin (TBT) in your tap water or residual pesticides on your vegetables. They’re finding microplastics in wild salmon. We’re all exposed to some pattern of obesogenic chemicals, which has altered how our bodies process the foods we consume.
This new, integrated model of obesity also makes it easy to think about things we otherwise take for granted, such as why people seem to think that metabolism is supposed to suddenly slow down in middle age. For my entire life, pretty much everyone I’ve known has walked around assuming that, at some point in middle age, metabolism supposed to magically slow down. The implicit assumption is that weight gain in middle age is a natural, normal consequence of getting older.
So then why doesn’t everyone gain weight in middle age? And why are more and more young children becoming obese? These changes have happened too quickly for genetics to be the excuse. If our environment is becoming more and more contaminated with obesogens, we’d expect obesity to rise everywhere, on average. At the same time, individuals are exposed to different patterns of obesogenic chemicals depending on their lifestyle and geographic location, and the underlying oxidative stress has a stochastic nature. People’s metabolisms will therefore break in different ways, at different rates. Thus, metabolic dysfunction becomes apparent for some in their 40s, some in their 30s, and others as children. Individual lifestyle differences and the stochastic nature of oxidative damage account for why metabolic dysfunction is simultaneously on the rise across demographics, but not every single person is getting gaining weight or becoming metabolically unhealthy at the same rate.
What’s even more alarming is that the obesogenic effects of certain chemicals can even be passed on form one generation to the next.
Obesogens & Epigenetics: the transgenerational inheritance of poor metabolic health
In M&M #145, I spoke with cell and developmental biologist Dr. Bruce Blumberg, whose lab is deciphering the biological mechanisms of obesogens. He described work that is unraveling how the environmental contaminant tributyltin (TBT) promotes obesity across generations.
In brief, if you expose male mice to TBT through drinking water, at doses equivalent to what some people have likely been exposed to, they become obese in response to only a modest change in their diet—a diet that does not result in obesity for control, non-TBT exposed mice. What’s more striking is that their offspring are also obese, despite the fact that TBT was not in their drinking water. The next generation of males is also obese, as is the one after that. That’s four generations of obese male mice, stemming from TBT-contaminated drinking water that was only ingested by the first generation. That would be like an American man today being obese because his great-great grandfather drank contaminated tap water.

How is this possible? How are subsequent generations of male mice able to inherit a phenotype a male ancestor acquired as an adult? That defies orthodox Darwinian thinking. If your dad lost an arm, that doesn’t mean his sons were born with one arm. In short, this can happen through epigenetic changes in sperm. TBT changes the structure of chromatin within sperm. The embryo formed by such a sperm cell has altered gene expression, ultimately resulting in a predisposition to diet-induced obesity in the the next generation. New evidence keeps emerging that diet-induced changes in the sperm epigenome can result in offspring inheriting the poor metabolic health of their parent.
All of the mechanistic details for this stuff are still being worked out. In my conversation with Dr. Blumberg, he described the TBT result mentioned above, as well as upcoming work which more clearly delineates how TBT induces its effects. In short, alters gene expression in ways that dysregulate the insulin secretion—despite eating the same diet as non-TBT exposed mice, those in the TBT-exposed lineage produce an exaggerated insulin response, promoting higher rates of adiposity and hence obesity.
TBT is one of many obesogenic environmental contaminants that humans have been exposed to. The amount of exposure you’ve had depends on your lifestyle and where you live. Given that many of the core biological mechanisms regulating metabolism are conserved across mammals, it’s likely that many obese humans have been exposed to significant levels of environmental obesogens like TBT. This may predispose their own children to obesity, even if they never directly ingest the same obesogens.
This phenomenon, the transgenerational epigenetic inheritance of poor metabolic health, is troubling in multiple ways. It suggests the possibility of parents passing on poor metabolic health to children, even if they were born metabolically healthy themselves. If subsequent generations are exposed to the same environmental obesogens and a poor diet, this could lead to compounding effects over time—a potential explanation for why obesity has continued rising over time despite increased physical activity and flat caloric intake. Given the ubiquity of obesogens in the modern world—microplastics, pesticides, food additives—it also suggests that complete avoidance is virtually impossible. The best you can do is mitigate the problem by avoiding pre-packaged foods, filtering your water, and so on. But even those efforts won’t be perfect.
Even if we could snap our fingers and remove all of the non-food, obesogenic contaminants in our environment, that still wouldn’t solve the obesity crisis. There is substantial genetic variation between people affecting how their bodies metabolize food. As a result, two different people fed the same diet, even if it’s devoid of all non-food obesogens, will process that food in different ways. Some would still become obese, gaining more weight than others for a given level of caloric intake.
Genetic Variation in Human Metabolism
How your body reacts to what you eat depends, in part, on your genes. There is substantial genetic variation between people in genes crucial for the metabolism of dietary macronutrients. This is why there is no universal human diet and some people stay lean while others gain weight despite similar diets and lifestyles.
One of the most well-known dietary phenotypes that displays strong variation among people is lactose tolerance. Like all mammals, humans are lactose tolerant early in life. After weaning, most mammals lose the ability to digest lactose. The gene encoding lactase, the enzyme which digests the lactose sugar, is pre-programmed to turn off after mother’s milk is no longer needed. Unlike most other primates and mammals, some human populations evolved lactase persistence—they acquired mutations in non-coding, regulatory DNA sequences governing when the lactase gene is expressed, enabling it to be expressed throughout adulthood.
Lactose tolerance arose in certain places, at certain times, in response to the domestication of animals that produce milk. Where this ability arose, it quickly spread through the population. When a genetic change spreads quickly, it indicates that is imparts a strong survival advantage. A good guess is that, among populations who had domesticated milk-producing animals, those with the ability to consume dairy as adults may have had a survival advantage in times of famine.
Because dairy animals were only domesticated in certain places, lactase persistence didn’t evolve everywhere. Where it did, it didn’t spread completely. This is why lactase persistence is only seen in about one-third of the human population today, and why its frequency varies some much across ethnicities.
As I learned from population geneticist Dr. Eske Willerslev in M&M #154, there is also substantial genetic variation in FADS genes, important for fat metabolism. FADS genes encode fatty acid desaturases, enzymes which transform saturated fatty acids into unsaturated fatty acids in the body, a process important for how our bodies handle dietary fats. Even among white Europeans, there is a lot of genetic variation in these genes, which arose in just the past 5,000 years due to natural selection. The specific versions of FADS genes that you have influences how you metabolize dietary fats, including how your LDL cholesterol levels change in response to the fatty acid content of your diet.
Recently evolved variation in other genes contributes to our risk of metabolic disorders like type II diabetes, as well as psychiatric conditions like Alzheimer’s (which some are calling, “type III diabetes”). The point is that there are inherent metabolic differences between people. All of us are some composite of different genetic lineages, each of which was partially adapted to particular diet and way of life. Whether you can tolerate lactose as an adult and what your cholesterol levels look like on a ketogenic vs. standard American diet depend on your genome. The way your genome can express itself is constrained by your ancestry—were your ancestors mostly Neolithic farmers adapting to a grain-based diet, Steppe Pastoralists eating a lot of meat and dairy, or hunter-gatherers from the tropics? The answer to that question is a major factor in how a given diet will affect you.
Eat less, move more?
For reasons that go beyond obesity, many people do need to eat less and move more. Let’s not lose sight of that. We did not evolve to sit around all day and eat as much as we want. There’s a reason why gluttony is one of the seven deadly sins, and all religions of long-lived cultures regulate food intake through fasting rituals and dietary taboos: because what you eat influences the type of person you become.
But the choices you make today are constrained in important ways by the brain you have, by a biological constitution the structure of which was sculpted by events from long before you started making choices. Substantial biological constraints were in place from the moment of fertilization—constraints that, in part, depended on both the genes and metabolic health of your parents at the time of conception. No matter what particular constraints you inherited, you were born into the modern world—a world filled with ultra-processed foods, environmental contaminants, and a deluge of sensory stimuli unlike anything our ancestors encountered.
“Eat less, move more,” can be suitable advice for some people, but it fundamentally can’t be the solution for everyone. Some people do eat less and move more, and still fail to lose weight because weight loss is not all about energy balance. Eat less? Of what? The specifics matter. You may have lost weight by cutting out refined grains, but the same diet and level of effort may fail for someone else—perhaps they’re descended from Neolithic farmers and you are not, or maybe their parents were exposed to more environmental obesogens than yours.
Human diversity is real and not merely skin deep. Our bodies do not react to what they’re fed in the same ways. There' is no one-size-fits-all lifestyle solution or universal mantra. Obesogens are seeping out of the modern environment we’ve built, affecting the biological source of the very will power we hope to summon. Unless you want to check out completely, move to wilderness, and write a manifesto, this is the world we inhabit.
What other options do we have?
One path forward is to adopt a philosophy of radical affirmation, positively embracing the hand life has dealt us. The environment is contaminated with obesogens and there’s not much we can do about it. Even if we could, I’m not giving up my potato chips—they taste great, and life is about satisfying our desires. Let’s embrace this way of life. Let’s be body positive: you are healthy and beautiful now matter what the state of your body is.
Many have taken this path:
Another path forward, which appears to be wildly popular: continue putting faith into the spirit of technological progress. Our environment may be poisoned, but the priests of Eli Lilly, Novo Nordisk, and our academic institutions will save us. They will create newer, better drugs that enable us to tolerate the poisons of modernity. The environment may be making us sick, but our saviors will invent new ways for us to endure it.
Is there another way? Or do we have to choose between embracing everything the world has become with Epicurean complacency and praying for some company to invent (and patent) a universal antidote for the poisons of modernity?
For most of human pre-history, people worshipped ancestor spirits. The will to move forward in this life was summoned through ritual and reverence for the unbroken chain of kinship we emerged from. Across most of human evolution, our ancestors had to struggle to survive, without the comforts we enjoy and in ways we can scarcely imagine. They also didn’t have to count calories, study nutrition facts, or neurotically engineer “protocols” into their weekly calendar.
We know a lot more about how the world and about biology than the peoples of traditional, pre-agricultural societies. And yet, without any of our modern knowledge, they had some things that we lack. Better mental health, without SSRIs. Better insulin sensitivity, without metformin. Good teeth, without dentists. Did they know something we don’t?
Perhaps the best path forward is to rely on the future, and await the Messianic arrival of Ozempic version 6.0, or whatever.
Or perhaps there are other paths, ones revealed by reflecting on the past and re-discovering things we once knew.

Related Podcasts:
M&M #140: Obesogens, Oxidative Stress, Dietary Sugars & Fats, Statins, Diabetes & the True Causes of Metabolic Dysfunction & Chronic Disease | Robert Lustig
M&M #145: Epigenetics, Hormones, Endocrine Disruptors, Microplastics, Xenoestrogens, Obesogens & Obesity, Inheritance of Acquired Characteristics | Bruce Blumberg
M&M #154: Evolution & Genetics of Human Diet, Metabolism, Disease Risk, Skin Color and Origins of Modern Europeans | Eske Willerslev
















Great reading. Thank you