Carbohydrate:Fat Ratios in Fat Gain & Obesity
Fat gain is sensitive to the ratio of consumed macronutrients like fats and carbohydrates. Confusion arises from simplistic focus on one nutrient at a time.
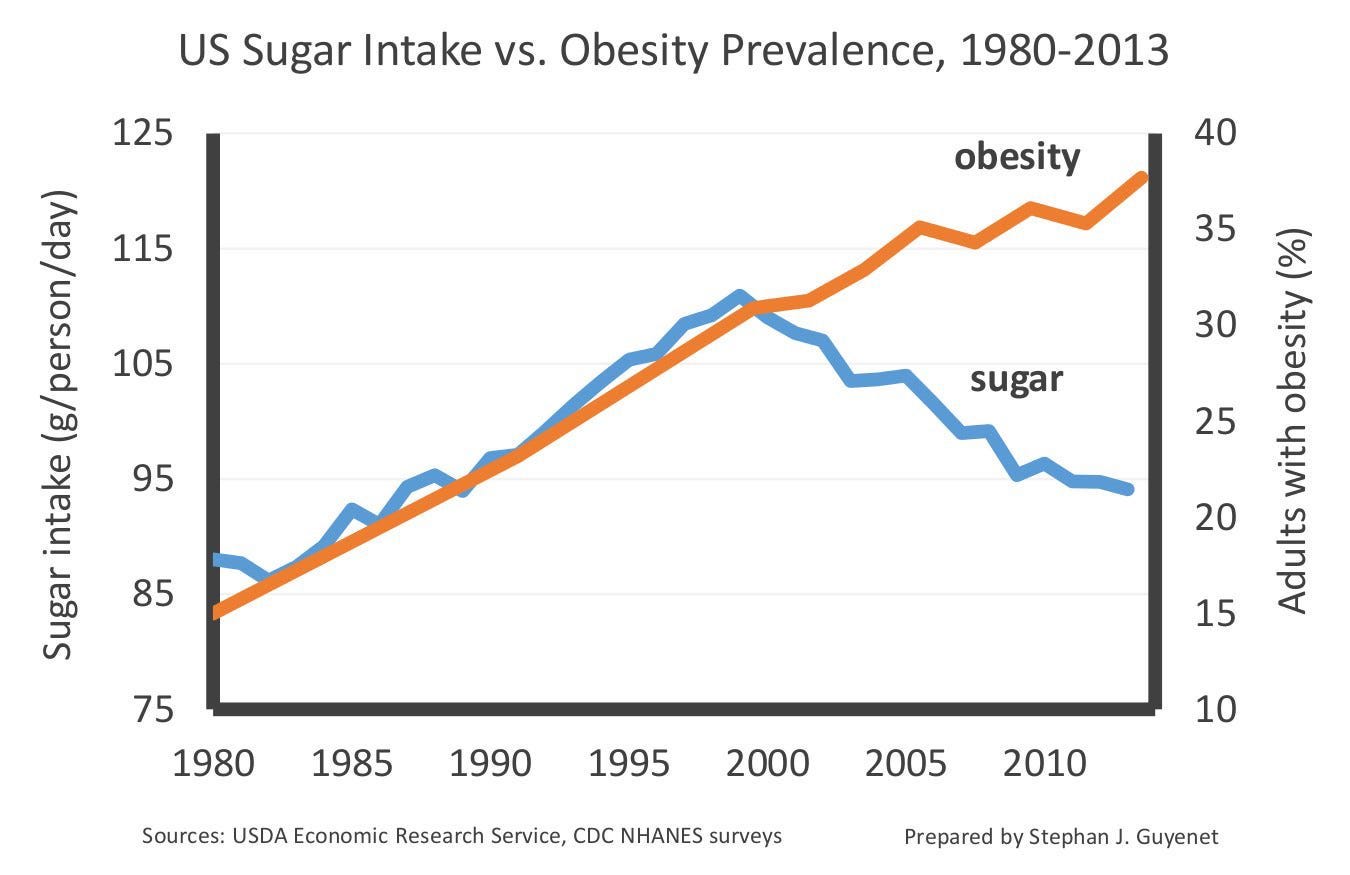
We previously looked at this graph, which appears to show a clear anti-correlation of sugar “intake” (the supply of sugar per capita) and obesity rates in the US:
While striking, there’s a lot we cannot know from this graph. Among other things, what if the drop in “intake”—which is really caloric sweetener availability, on average—is driven mostly by, say, 10% of the population who started diligently avoiding added sugars at all costs? It’s impossible to know exactly how this drop maps to the population. What we can say for sure is that it’s definitely not true that everyone started reducing sugar intake to the same degree, at the same time. In any case, the point we made last time was that perspective matters:
In this article, I pointed out that the relationship between two individual variables can appear very different when you’re zoomed in or out, and then pretty much just said that biology is complicated and we shouldn’t jump to conclusions about sugar and obesity from data visualizations like this. The fact remains: obesity rates continued climbing since 2000, despite drops in average sugar availability. The drop may be small in the full context of its massive historical surge since the 1800s, but it ain’t nothin.
Is it possible that sugar intake could be an important factor in the rise in obesity, and also that we should expect obesity rates to have continued climbing despite a decrease in sugar intake? Are there any biological reasons for why this could be true, and we should therefore not jump to conclusions about sugar and obesity from this population-level data alone?
The answer to those questions is, “Yes.”
Let’s dissect the issue through the lens of macronutrient ratios, just one angle this topic can be analyzed from. Altering the carbohydrate:fat ratio can have drastic effects on adiposity (fat gain) and metabolic health more generally. Macronutrients ratios can even be a more potent driver of certain physiological effects than total caloric consumption. This opens the possibility that, under some conditions, a drop in the intake of one macronutrient can shift nutrient ratios in a way that drives more adiposity despite a decrease in overall caloric intake.
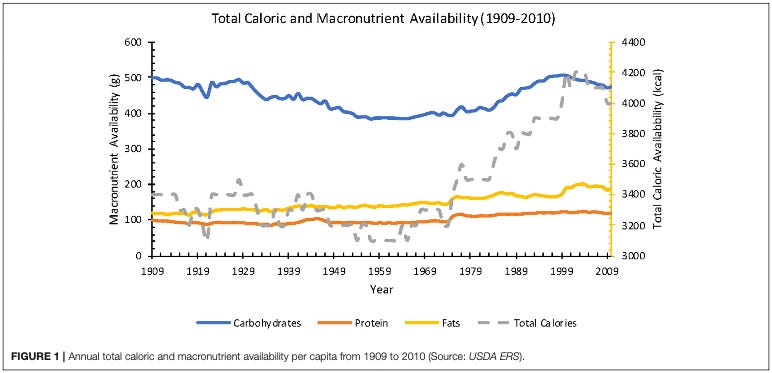
But first, let’s crunch some numbers. How has the ratio of macronutrient availability—the relative abundance of fat, carbohydrate, and protein—in the American diet changed over time? Let’s create a rough map of those changes before diving into the biology of macronutrient ratios and adiposity.
American Macronutrients: the carb:fat ratio over time
If we eyeball our caloric sweetener graph, we can see that supply was roughly flat for a number of years after WWII, rising modestly after 1960 and then sharply around 1980. Things peaked in 2000, before dropping down to levels that were still higher in the early 2010s than they were before the 90s. From that peak, supply dropped approximately 10-15% by 2016. Remember: this is a graph of supply, not intake per se. It also only covers caloric sweeteners, not all forms of sugar or carbohydrate.
If we look at CDC data from the 1970s onward, into the 2015-2018 period, we see a similar pattern for estimates of overall carbohydrate intake:
1971-1974 | carb:fat:protein ~44:37:17 | carb:fat = 1.2
1976-1980 | carb:fat:protein ~45:37:16 | carb:fat = 1.2
1988-1994 | carb:fat:protein ~50:34:15 | carb:fat = 1.5
1999-2000 | carb:fat:protein ~51:33:16 | carb:fat = 1.5
2015-2018 | carb:fat:protein ~47:36:16 | carb:fat = 1.3
The carb:fat:protein numbers are the percentage of calories from each macronutrient class (rounded and averaged, which is why they don’t exactly sum to 100). As with caloric sweetener supply, the percent calories from carbohydrates began rising by the late 1980s, peaked in 1999-2000, then dropped down to levels a little above where they were before the spike.
The trend for overall carb intake mirrors that for caloric sweeteners: from the 1970s to 2016 carbohydrate intake rose, then peaked, then fell. All the while, obesity continued rising. Should we jump to the conclusion that carb intake isn’t a factor in obesity?
Nope.
The spike in caloric sweetener supply looks dramatic if the plot starts at 1970-80, but zooming out to see data going back ~200 years reveals it to be a more modest change. This pattern is also seen for total calorie and total fat availability, as well as specific dietary fats:
Total calorie and fat availability “spiked” in 1999-2000, but still remained above historical levels after dropping from their peak. Notice also that polyunsaturated fatty acids (PUFAs, i.e. seed oils) defy this pattern, rising steadily into the 2000s and remaining at or near all-time highs to the present. Even though the consumption of carbohydrates and caloric sweeteners has dropped since 2000, this co-occurred with an increase in PUFA (seed oil) consumption.
PUFAs like linoleic acid are obesogenic in animal models. Reducing the linoleic acid content of high-fat diets can reverse their obesogenic properties. If multiple nutrients have obesogenic effects, the obesogenic effects of one can be masked by the rise in another—yet another reason why looking at high-level, population-wide data like this should be done with caution.
To learn more about the evolution of the human diet, try these M&M episodes:
M&M #135: History of Diet Trends & Medical Advice in the US, Fat & Cholesterol, Seed Oils, Processed Food, Ketogenic Diet, Can We Trust Public Health Institutions? | Orrin Devinsky
M&M #136: Seed Oils, Omega-6 PUFAs, Inflammation, Obesity, Diabetes, Chronic Disease & Metabolic Dysfunction | Chris Knobbe
Look again at the macronutrient data trends above, but focus on what has not changed since the 1970s:
Carbohydrates have always been ~45% or more of available calories.
Fats have always been more than ~33% of available calories.
The carb:fat ratio has stayed within 1.2 - 1.5, biased toward carbs.
Protein availability has remained approximately constant, at ~16% of calories.
Over this entire interval, the average American has been getting a third or more of their calories from fats and more than one-third from carbohydrates, on a background of steady protein intake (assuming supply faithfully reflects intake). Despite the modest dip in carbohydrate intake since 2000, Americans are still getting almost half of their calories from carbohydrates. After 2000, the carb:fat ratio dropped, but to a level still higher than it was prior to the 1980s.
The carb:fat ratio decreased, but it moved closer to 1:1. This happens to be the balance of fat and carbohydrate intake that is often the most effective at driving adiposity in animals…
Nutrient Ratios & Adiposity
It should be fairly intuitive why the relative balance of nutrients has important metabolic effects. Every cell in our body will pretty much utilize all of the nutrients available to it, to some extent or another. Micronutrients like vitamins often serve as cofactors that “help” enzymes, which are built out of the amino acids we acquire from dietary protein, which influence the digestion of carbohydrates and fatty acids, etc., etc., etc. Layer upon layer of interdependency.
Cells can even engage in metabolic switching, changing their mode of energy mobilization in response to available energy sources. For example, certain forms of dietary restriction, such as extended fasting or a substantial reduction in carbohydrate intake, can trigger the body to begin using fat as it’s primary energy source. The state of “ketosis” that follows ultra-low carbohydrate consumption represents a metabolic shift away from carb metabolism—individual cells reconfigure their internal workings, dialing up or down different sub-cellular mechanisms in order to adapt to the materials they’re given to work with. These reconfigurations are a response to changes in the relative abundance of nutrients like fats and carbs.
If you enjoy this content, try these M&M articles:
Sugar Has No Impact On Obesity: Just-so stories in metabolic health
The influence of fat:carb ratios on adiposity: animal research
Use of “high-fat” diets is pervasive in animal research. Multiple versions exist, but researchers typically order standardized “high-fat” chow from large suppliers. “High-fat” chow does indeed contain more fat than the standard chow used by default, but also typically contains significant levels of carbohydrate. High-fat chow will often contain ~60% of calories of fat (give or take), but also 20-50% from combinations of refined carbohydrates like corn-starch, maltodextrin, sucrose.
Among studies where the fat and carb content is specifically known and probed as a variable, there are many examples showing that the obesogenic effects of diets are sensitive to the overall fat:carb balance. Here are some example referenced in this review paper (lightly paraphrased):
Diets fed ad libitum that provide most calories as fat, but lack carbohydrate, typically do not induce obesity in laboratory rodents. However, adding a small amount of carbohydrate (as low as 3–4% by weight) will make such high-fat diets obesogenic.
Dietary carbohydrates (i.e. starch or sucrose), not fats, may drive both the increased fat accumulation and hypothalamic inflammation associated with consumption of long-chain saturated fat diets in mice.
“High-fat” diets with equicaloric proportions of carbs and fats (~40% each) appear most effective in causing excess fat deposition compared with diets matched for caloric density but differing in the proportion of carbs and fats.
Fat accumulation and feed efficiency decline as this ratio diverges from parity in favor of either macronutrient, consistent with a primary metabolic effect of dietary composition that shifts the flux of fuels toward storage.
One specific study I’ll highlight gave mice diets composed of 20% protein, with variable amounts of fat and carbs. Across several isocaloric diets which differed in fat-carb balance, diets close to a 1:1 ratio drove the most weight gain and fat mass:
This effect held whether the primary carbohydrate source was sugar (sucrose) or cornstarch:
Now recall the drop in American sugar supply (“intake”) we originally considered, together with the change in the overall carb:fat ratio. Presumed sugar intake dropped from the year 2000 onward, with the carb:fat ratio declining from 1.5 to 1.3. This is almost exactly the carb-fat balance that was most effective at driving weight and fat gain in mice. And all of that was on a backdrop of historically elevated caloric intake, fat and carbohydrate each contributing to more than one-third of American calories, and PUFA consumption rising the whole time.
Again, we are not making any definitive claims here about why obesity has continued rising since 2000. We are simply highlighting one of many reasons why we cannot dismiss sugar intake as playing a role in the obesity epidemic by looking at one proxy measure of intake going down. It’s entirely possible that typical American diets remained obesogenic despite any real declines in caloric sweetener intake, just considering the carb:fat ratio (which isn’t the only thing worth considering).
To point you to just one more relevant dimension to the story of modern obesity, it’s entirely possible that, for over a century, each new generation of Americans has become more prone to the obesogenic effects of our diet due to exposure to metabolism-disrupting chemicals in utero and throughout life—chemicals which can, for example, screw up insulin signaling so that food intake drives more adiposity than it otherwise would. All of us have probably been exposed to varying levels of obesogenic environmental toxins to some extent. Our great grandparents may have eaten similar levels of carbohydrate and fat compared to us (maybe), but they were not consuming the same form factors, ingesting nearly as many non-nutritive additives, or marinating in as many synthetic endocrine disruptors or SSRIs in the womb.
Sticking with the subject of carb-fat balance, it’s worth considering how this has varied across time and space for human populations.
Diets with distinct carb:fat ratios around the world
There is no question that the “Standard American Diet” is very fattening. Many of us lived through the “low-fat” craze of the 1980s and 90s. For some strange reason, whole grain Cheerios, unlimited Olive Garden breadsticks, and our choice of low-fat salad dressings at the Ponderosa buffet didn’t make American healthy again. Why? Maybe it’s all the refined carbohydrate. Some people blame seed oils. Whatever the major factors are, there’s certainly more than one of them. Don’t lose sight of that.
Here’s the supply graph we looked at before (again, this not a graph of actual intake):
Based on the estimates of intake from CDC data, we saw that the carb:fat ratio has been between about 1.2 and 1.5 since the 1970s. This means that, despite being fattening, it would be misleading to call this a “high-fat” diet, as it contains more carbs than fat. It would be fair to call it a high-fat and high-carb diet, or something similar. The typical American is consuming a substantial amount of their calories from carbs and a substantial amount from fats, in something approaching a 1:1 ratio of the two.
In the mouse data we looked at above, C45:F35 diets—slightly biased toward carbs, just like the average American diet—were most effective at driving weight and fat gain. When the carb-fat balance deviated from this substantially, in either direction, mice were leaner. This observation in mice is evocative of patterns we see in the ethnographic record, with human hunter-gatherers eating diets skewed heavily towards fats and away from carbs, or vice versa.
In this article about dietary fatty acids, I mentioned two traditional populations whose diets have substantially different macronutrient profiles, but from each other and compared to present-day Americans. The traditional Inuit diet was about 8% carbohydrate, whereas native Papua New Guineas have a staggering 95% carbohydrate diet. The Standard American Diet contains less fat than the Inuit diet, less carbohydrate than Papua New Guinean diet. Perhaps one reason why the American diet is so fattening is that it’s both high-fat and high-carb, with comparable levels of each.
There are of course many other differences between these diets, beyond the raw fat and carbohydrate content. But the specific balance of fat, carbohydrate, and protein is an important factor determining the obesogenic potential of animal diet. Macronutrient ratios likely influence many aspects of health. Some evidence even suggests that these ratios can be more important than overall caloric intake in overall cardiometabolic health.
In terms of the carb:fat ratio, a key take away from what we’ve seen here is that weight and fat loss could very well be least effective when your intake of fat and carbohydrate are both in the 30-50% range—exactly the range that most Americans have been stuck in for decades and decades, and perhaps why more and more people seem to be finding success with “extreme,” ultra-low-carb ketogenic and carnivore diets.
At the end of the day, there is no population-level food supply data, mechanistic laboratory rodent study, or even randomized, double-blind, placebo-controlled human clinical trial that will provide definitive, unassailable information about how your body will respond to a given change in diet. You’re an, “n of one” (n=1). Making changes to your diet—being diligent about what, how, and when you eat—is the best way for you to understand how what you consume changes who you are.
If you want to shed some fat, experiment with your diet. But it may not be enough to cut back on fat a little bit, or decrease carb intake somewhat. To see substantial changes in your body it may be necessary to first make effortful changes to how you focus your mind.
Of course there are now alternative approaches, which require less volition—just ask a physician about Ozempic or one of the other new GLP-1 drugs. You will be able to enjoy all of the same junk you ate before, while you were putting on the weight. You’ll just eat less of it. It may even help you quit drinking. But don’t come crying to the rest of us if it turns out to be Rimonabant 2.0. It will probably take a few years before we know the answer to that one for sure. In the meantime: decisions, decisions…
To learn more about subjects covered in this article, see these scientific papers and M&M podcast episodes:
Macronutrient ratios in health & disease:
PDF: The Ratio of Macronutrients, Not Caloric Intake, Dictates Cardiometabolic Health, Aging, and Longevity in Ad Libitum-Fed Mice
M&M #132: Obesity Epidemic, Diet, Metabolism, Saturated Fat vs. PUFAs, Energy Expenditure, Weight Gain & Feeding Behavior | John Speakman
M&M #106: Diet, Macronutrients, Micronutrients, Taste, Whole vs. Processed Food, Obesity & Weight Loss, Comparative Biology of Feeding Behavior | Stephen Simpson & David Raubenheimer
Biology regulation of body fat, adiposity & GLP-1 drugs
Obesogens & environmental toxins in metabolic dysfunction











I have seen blogs (Brad Marshall) that American diet was very carb heavy in early 1900 and presumably before.
Since, then starch has gone down quite a bit but sugar has increased. Sugar intake in 1900 was not trivial.
In Europe too, carb intake was heavy in pre-industrial period.
One can derive the hypothesis that obesity is correlated with fat intake.