Sugar Has No Impact On Obesity: Just-so stories in metabolic health
In a world overflowing with data, it's easier than ever to construct "just-so stories" around our preferred conclusions
Not medical advice.
Confession: I don’t believe this.
Sugar intake has almost certainly played an important role, as one contributing factor, in the modern epidemic of obesity and metabolic dysfunction. “Sugar” is too vague to reason clearly here. There are multiple considerations obscured by that generic term: the specific types of sugars you consume, form factor, pattern and frequency of consumption, nutrient ratios, etc. And that’s sugars, plural—there are different types of sugars (e.g. glucose vs. fructose), each of which has different metabolic effects. All of that complexity is layered on top of even more, some of which is independent of consumptive behavior: genetic background, family health history, exposure to metabolism-disrupting chemicals.
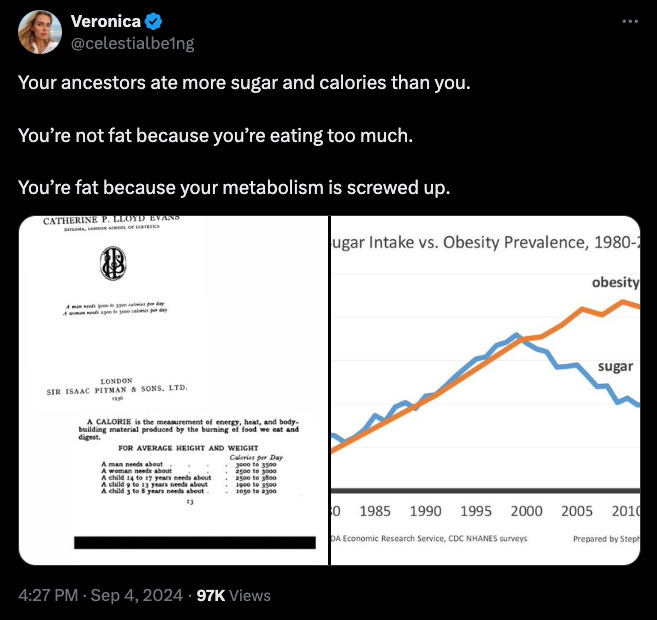
Confronted with complexity, we naturally seek to simplify. Everyone loves an elegant theory. From the desire to simplify and achieve certainty, people often fall prey to various sins of reasoning and argumentation, ranging from honest mistakes (e.g. not realizing other evidence exists) to the deliberate misrepresentation of data. Entire fields of study, such as nutrition epidemiology, are built on a foundation of shoddy data. The modern information environment—a world overflowing with anecdotes, data, and scientific studies of highly variable quality—makes it easier than ever for people to construct “just-so stories.” What’s especially troubling about the present-day is that such stories are not pure fiction, pulled out of thin air. They often contain graphs, citations, and p-values. Every year, we hear about more and more high-profile research retractions, including work by Nobel winners cited hundreds of times each.
Technology keeps improving. More and more studies published. New LLMs gorging on text as we march toward AGI.
All of that, and yet: the line between fact and fiction seems to be getting blurrier.
Three common behaviors often seen in people who have become emotionally attached to their favored explanation for complex phenomena:
Misinterpretation and/or misrepresentation of real data, often with a narrow focus on single-variable interactions when many interacting factors are at play.
Cherry-picking observations that support the desired conclusion while ignoring important contextual factors.
Generalizing from limited sample sets or personal experience.
This post isn’t be about coming to a conclusive stance about the precise role sugar intake has played in obesity. Instead, we will use this issue to illustrate how easy it is the construct just-so stories in the realm of diet and metabolism. We want to get better at spotting these behaviors in order to inoculate ourselves from falling victim. Doing this will nonetheless reveal many important things about sugar metabolism and its relationship to obesity, including reasons why I believe it is one significant variable in the obesity epidemic.
Biology is complicated. Total certainty in “the truth” is never guaranteed. We must become comfortable with uncertainty in order to avoid becoming religiously devoted to our favorite ideas. People love that fuzzy feeling of certainty, of believing we are among the enlightened few who “get it.” Peoples of the past knew the dangers of this addiction: “Ἐγγύα πάρα δ Ἄτα” (Certainty brings insanity)
Below I will construct an evidence-based argument for why sugar intake has nothing to do with obesity—then we’ll tear it apart, showing how it rests on the three misbehaviors listed above. My aim is to emulate real-world arguments, using presentations of data and evidence commonly used in social interactions. Just to be clear: we will be reasoning poorly, starting with a conclusion and then using available evidence to construct a just-so story.
Just-so: Obesity has nothing to do with sugar
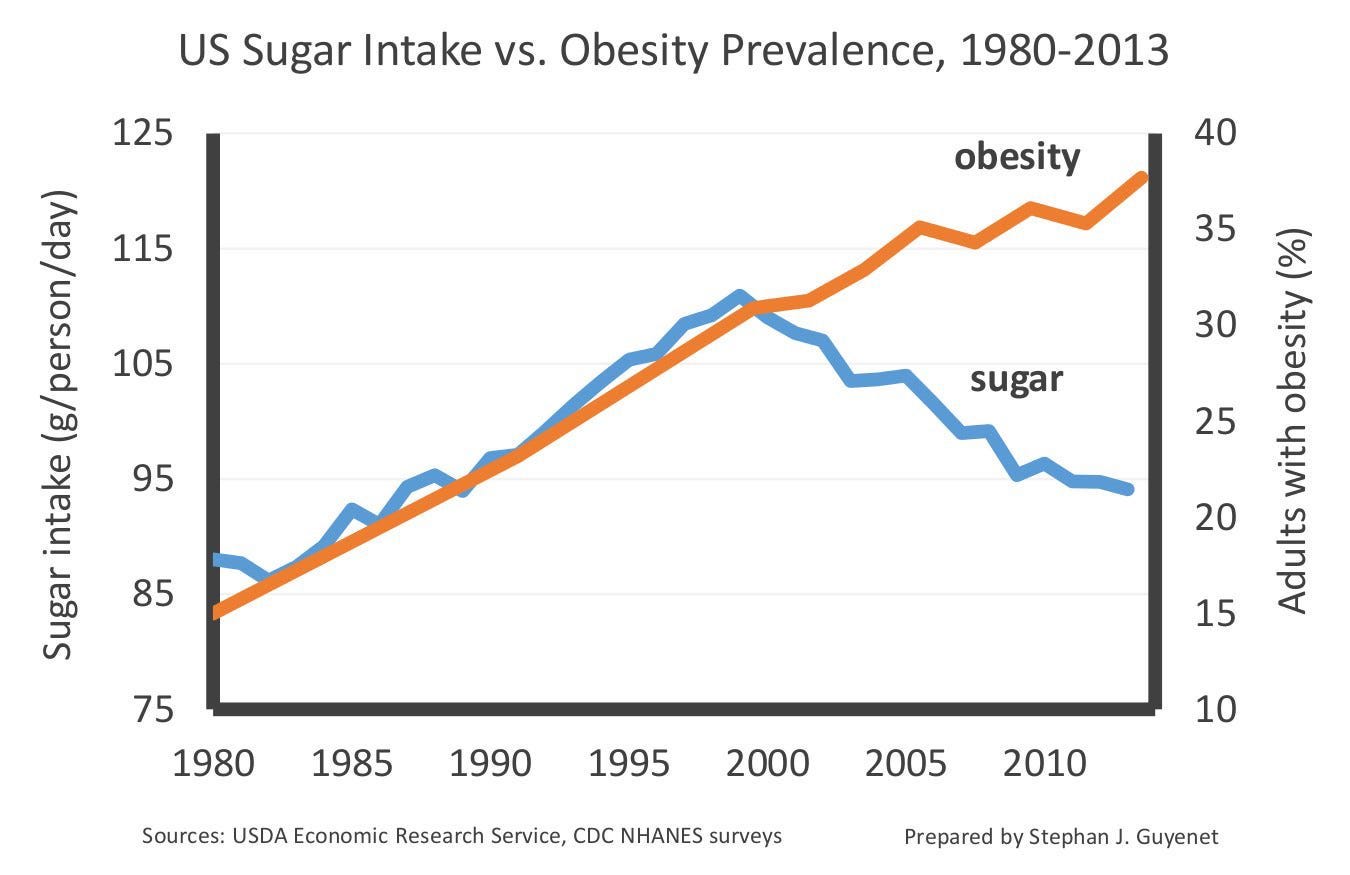
If sugar intake was a significant factor in driving obesity rates, we would expect to see a clear correlation between these two variables. Correlation doesn’t prove causation, but the lack of correlation does indicate lack of causation (assuming your data are accurate). Looking at data on sugar availability vs. obesity rates going back over three decades, we see this:
What’s most striking is that since the year 2000 sugar intake declined for years while obesity kept on rising. The two variables are anti-correlated in the time period, opposite to what we’d expect if sugar was obesogenic. At the very least, we should have seen obesity rates level off (i.e. increase less) after sugar intake dropped. But we didn’t.
This anti-correlation seen in data from the US fits with patterns we see in traditional human societies. Diets rich in sugar are common in the ethnographic record, especially among hunter-gatherers native to tropical and temperate climates. In some populations, honey intake alone accounts for 10-20% of annual caloric intake. For example, the Hadza people of Tanzania consume honey and berries year-round. Depending on the month, a majority of their total calories can be derived from one or both of these natural sources of sugar.
There is evidence that honey has been a food source for species in the genus Homo for roughly three million years (see the reference in the figure below for more detail). Other great apes regularly forage for honey. Collectively, these observations suggest that sugar-rich foods have been staples of human diets for as long as our species has existed (at least for some populations). But the obesity and metabolic dysfunction often attributed to sugar consumption are hyper-modern phenomena, rarely seen in traditional populations. The Hadza seem to have excellent metabolic health. If high sugar consumption was a major driver of obesity, then why are the Hadza people lean and healthy?

To learn more about the evolution of the human diet, try these M&M episodes:
Podcast: Diet, Hunting, Culture and Evolution of Paleolithic Humans & Hunter Gatherers | Eugene Morin
Podcast: Ancestral vs. Modern Human Diets, Seed Oils, Inflammation, Fat Oxidation, Influence of Industry on Food Science | Steven Rofrano
The absence of metabolic disease in people eating high-sugar diets is not limited to hunter-gatherers—there are many examples of modern, Western people who consciously eat hundreds of grams of sugar per day. Such individuals not only fail to reliably develop obesity and other metabolic issues, some even claim that they’ve reversed metabolic dysfunction (and other problems) after starting a high-sugar diet:
Many such people identify as “Peaters,” those whose diets are inspired by the late Dr. Ray Peat, a maverick physiologist known for his unconventional ideas related to diet and metabolism. Peaters routinely report consuming hundreds of grams of sugar per day from natural sources like fruits and honey. Not only does this community seem to report low rates of obesity and metabolic dysfunction, but many report the exact opposite: reversal of dysfunction and abundant energy levels once they adopted a Ray Peat-style high-sugar diet.
(Side note: people in the diet & metabolic health discourse can be passionately devoted to their “tribe,” sometimes to the point of cultishness. To help avoid being dismissed as an “anti-Peater” by some, let me say that I have much respect for the late Dr. Peat, an independent thinker whose ideas should be carefully considered. He was also one guy. In my life, I’ve yet to come across a single person who was always right, about everything. This post should not be mistaken for an anti-Peat diatribe.)
If regular, high sugar intake was a major factor in obesity and metabolic dysfunction, we would expect Peaters to be disproportionately obese and metabolically unhealthy. But that doesn’t appear to be the case, at least from what we see posted by self-proclaimed Peaters online. 400-500 grams of daily sugar intake is a lot. It’s not difficult to find such reports. Such reports appear genuine, and the transformations people experience turn them into enthusiastic evangelists of this dietary approach.
To summarize the main argument:
In recent history, there is an anti-correlation between sugar intake and obesity—sugar consumption and obesity rates seem to be moving in opposite directions.
Humans have a long evolutionary history with sugar-rich foods like honey. Human hunter-gatherers who get a majority of their calories from sugar are nonetheless lean and metabolically healthy.
A subset of people in the modern, Western world report being lean and metabolically healthy despite consuming hundreds of grams of sugar daily. Some even report reversing metabolic dysfunction with such a diet.
How can one possibly think that sugar intake is a significant factor in the modern obesity epidemic given this set of observations?
Deconstructing the argument
Recall the three sins of reasoning pointed out previously:
Misinterpretation and/or misrepresentation of real data, often with a narrow focus on single-variable interactions when many interacting factors are at play.
Cherry-picking observations that support the desired conclusion while ignoring important contextual factors or counter-examples.
Over-generalizing from limited sample sets or personal experience.
Let’s now deconstruct the above argument step-by-step, keeping these misbehaviors in mind. I’ll split the full chain of reasoning into three segments.
Argument #1: Sugar intake and obesity are anti-correlated
Recall the graph above:
A striking pattern indeed.
If this chart was providing a comprehensive picture of reality, it would be reasonable to conclude sugar isn’t an important dietary factor in obesity. But this data is not comprehensive—it’s misleading, with the graph presented in a way that makes a specific micro-pattern look much larger than it really is.
It is not at all surprising that obesity rates have continued to climb since 2000 despite those apparent drops in average sugar intake. To begin to see this, we need to zoom out:
The physicist Richard Feynman famously said that the first principle of science is, “You must not fool yourself, and you are the easiest person to fool.”
See how the first presentation of the graph we looked at enables us to fool ourselves? We saw sugar intake only from 1980 onward. When we look at the data going back to the 1800s, a different picture emerges: the drop starting in 2000 is tiny compared to the massive rise in that went on for over a century. The strength and direction of a correlation can depend heavily on how much of the total available data you consider.
Pro-tip: always pay close attention to the axes of graphs, and consider whether the x- or y-axis are truncated. Axis truncation enables one to “zoom in” on data trends. This can be helpful, as when the zoom-in is shown directly alongside a non-truncated version (as in the example just above). However, if all you see is the truncated version, it’s easier to fool yourself.
If you’re interested in learning more about trends in the US food supply over time, check out my discussion with Dr. Orrin Devinsky:
M&M #135: History of Diet Trends & Medical Advice in the US, Fat & Cholesterol, Seed Oils, Processed Food, Ketogenic Diet, Can We Trust Public Health Institutions?
Also important: this is not a graph of actual sugar intake. The chart is showing us the total supply, a proxy for intake. While supply and intake are presumably well-correlated, it’s hard to know just how precisely. We therefore need to proceed with caution when interpreting this graph. Does a 10% drop in supply equate to a 10% drop in average consumption? Even if it does, is that significant in the context of a severalfold increase in supply since the 1800s?
With this more complete view of historical trends, we can see that it’s misleading to point to declines in sugar supply in the early 2000s and conclude that sugar intake has nothing to do with obesity. This is a misrepresentation of the true overall pattern.
Again, I’m not aware of anyone serious who claims that sugar intake alone can explain the obesity epidemic. I’ve talked to plenty of people who say it’s an important factor (e.g. Robert Lustig, Gary Taubes, etc.), but not anyone who says it’s the whole story. In contrast, I have seen people use the truncated graph above to argue that sugar intake has little or nothing to do with obesity…
Argument #2: Hunter-gatherers and past humans ate more sugar than you, but were lean and metabolically healthy
The third point above is correct: many people have a screwy metabolism. But to suggest that obesity and weight gain have nothing to do with total calorie or sugar consumption is off the mark. That conclusion simply doesn’t follow from the truncated graph being pointing to.
The full sugar supply chart above shows that, on average, Americans may have consumed fewer calories and less sugar twenty years ago (one generation) than they are today. And it’s plausible that health-conscious people like you or me might be consuming less than our parents or grandparents. But this is not the case if we compare ourselves to people living 200 or 20,000 years ago. There may be niche exceptions to this, but unless you’re descended from the Hadza tribe or have been going out of your way to eat massive amounts of honey or whatever, the vast majority of your ancestors were consuming fewer calories and less sugar.
Hunter-gatherers like the Hadza may eat lots of sugar, but they’re not consuming sugar as Westerners do. They actively expend energy—climbing tall trees, fighting off bees—to obtain raw honey. It’s consumed honeycomb and all, including protein-rich bee larvae. They’re not sitting around sipping on store-bought corn syrup. Climbing baobab trees to gather and eat raw honey will not have the same metabolic effect as drinking an equicaloric amount of Dr. Pepper.
People commonly cherry-pick from the anthropological record to make sweeping claims about all humans. “Sugar can’t possibly be a factor in driving metabolic dysfunction—the Hadza eat lots of honey but they’re lean and healthy!”). Comparisons of different human groups can be instructive, but it’s easy to abuse to anthropological record given the diverse range of past and present human cultures one can cherry-pick from.

Argument #3: You can be lean and metabolically healthy on a high sugar diet
I have no dispute with this claim in principle. I believe there are people who can consume hundreds of grams of sugar per day without becoming obese, depending on the specific forms of sugar they consume, energy expenditure, genetic factors, etc. The problem here comes when we generalize from individual cases of high-sugar consumption to the entire population while ignoring critical contextual factors: the volume of specific types of sugar consumed, the foods and forms factors they’re consumed from, pattern and frequency of consumption, and so on.
The Hadza example above offers a good starting point. These people do eat a lot of sugar. But a Hadza boy climbing baobab trees is leading a very different lifestyle than these hyper-sedentary Western kids:
Even if sugar intake was matched gram-for-gram, the metabolic effects of each diet-lifestyle combination would produce distinct health effects. The Hadza boy spends much of his day running and climbing in a semi-tropical environment, eating raw honey containing not just simple sugars like glucose and fructose, but waxes from the honeycomb and even protein-rich bee larvae. The boys at Micky D’s are drinking liquid corn syrup while eating starch deep-fried in soybean oil.
One of the overarching points here is that biological context must always be carefully considered, especially when we’re making comparisons between individuals and populations. Just consider the dramatic ways that the populations we’ve mentioned differ: the Hadza hunter-gatherers leading a traditional lifestyle in Africa, the hyper-health conscious Peater measuring their sugar intake down to the nearest gram, and the obese Western child drinking carbonated sugar water by the liter.
The Hadza person and Ray Peat fanatic both eat hundreds of grams of sugar from honey and fruit per day. The former does so by effortlessly participating in their traditional culture. The latter has spent countless hours reading about metabolic health and trial-and-erroring their diet in order to engineer a high-sugar diet (mainly from whole foods). Neither of these two lead the sedentary lifestyle of the obese Western child. And none of these three is consuming the same cocktail of sugars and carbohydrates—all are consuming sugars in different ratios, from different food sources, with different patterns and frequencies of consumption.
It is not sensible to point to the leanness of any one person or group consuming a high-sugar diet, and conclude from their existence that “sugar” is not a significant factor in the modern obesity epidemic.
If you enjoy this content, try these M&M articles:
Biological context & multivariate problems
All of this is meant to call attention to the myriad contextual variables at play here. Just because one type of person or one traditional culture stays lean and metabolically healthy by eating high levels of certain sugars, within a certain lifestyle context, it does not follow that “sugar” has nothing to do with the obesity epidemic ravaging the modern, Western world.
There are many examples in biology where a single factor makes a causal contribution to some outcome, but only in the right context—only when the right constellation of other, interacting variables are present. The entire field of genetics is filled with examples. Many variations of single genes exist which contribute to the development of a disease, but only in the presence of other genetic variants or when the right environmental variables impinge on the organism. This is why we usually say that variants “modifies disease risk,” rather than causing the disease full-stop. For example, there are gene variants clearly tied to your risk of developing breast cancer, such as alleles of BRCA1/2. Having those variants does not automatically mean you will get breast cancer, however. The overall risk depends on the presence of other gene variants (e.g. p53 tumor-suppressor variants) and various environmental factors (e.g. reproductive history, hormone therapy, etc). Lots of people who possess “disease-promoting” variants of BRCA nonetheless never develop breast cancer. The existence of such individuals does not negate the causal involvement of those variants in breast cancer development.

To begin to understand the relationship between sugars, obesity, and metabolic health more generally, we should discard “sugar” as an umbrella term, as if it refers to the same thing in all contexts. We need to think at the level of specific sugar types, carefully considering things like:
Distinct metabolic effects of simple sugars like glucose vs. fructose.
Form factor in which specific sugars are consumed (e.g. liquid or solid, with or without fiber).
Reinforcing properties of different sugars and how these relate to patterns of consumption.
Developmental timing of obesogen exposure & transgenerational effects.
The ratio of sugars and carbohydrates to other macronutrients.
Unpacking the details within each of these points is beyond the scope of this post. For now, I will leave you with some scientific papers and M&M podcast episodes relevant to four bullet points above.
Be careful: the more you learn, the more raw material you have to construct just so stories.
Distinct metabolic effects of fructose vs. glucose:
Influence of form factor (e.g. fiber presence) on the metabolic effects of sugars:
Reinforcing properties of glucose and fructose
PDF: Sugar Addiction: From Evolution to Revolution
M&M #184: Coming soon…
Developmental & transgenerational effects of obesogen exposure:
Role of macronutrient ratios in metabolic health outcomes









This is the most nuanced and well thought out take on sugar I’ve seen; thank you for writing it. I agree with almost everything here. I suspect that even if some part of diet Twitter were to figure out a relatively complete solution to diabesity (~98 percent of the population can eat to satiety and have great energy levels, bmi, and metabolic health when eating within the bounds of this solution) it will be too complex to be practically implemented throughout society without some sort of top down controls,
I’d also like to emphasize that there probably are certain phenotypes of person whom can eat very high sugar diets, and given the correct conditions (low pufa, potentially low fat in general) and have great outcomes.
I’m interested to see how the honey diet performs long term. Short term it’s a slam dunk for many, but perhaps it will form some long term health problems.